If you’re living with urethral prolapse, you know that it can significantly affect your daily life, causing discomfort and various urinary issues.
As a physical therapist with years of experience in pelvic health, I’ve seen firsthand how challenging this condition can be. Fortunately, with the right knowledge and proactive approach, managing urethral prolapse and feeling better is entirely possible.
In this article, we’ll explore urethral prolapse, its classifications, causes, symptoms, and the best treatment options to help you control your health.
What is Urethral Prolapse?
Urethral prolapse, also known as urethrocele, is a condition where the urethra, the tube that carries urine out of the body, either pushes into the vaginal canal or sticks out through the urethral opening.
This is more common in females but can also happen in men, though it’s much rarer. In men, it usually means the inner lining protrudes through the external opening of the urethra.
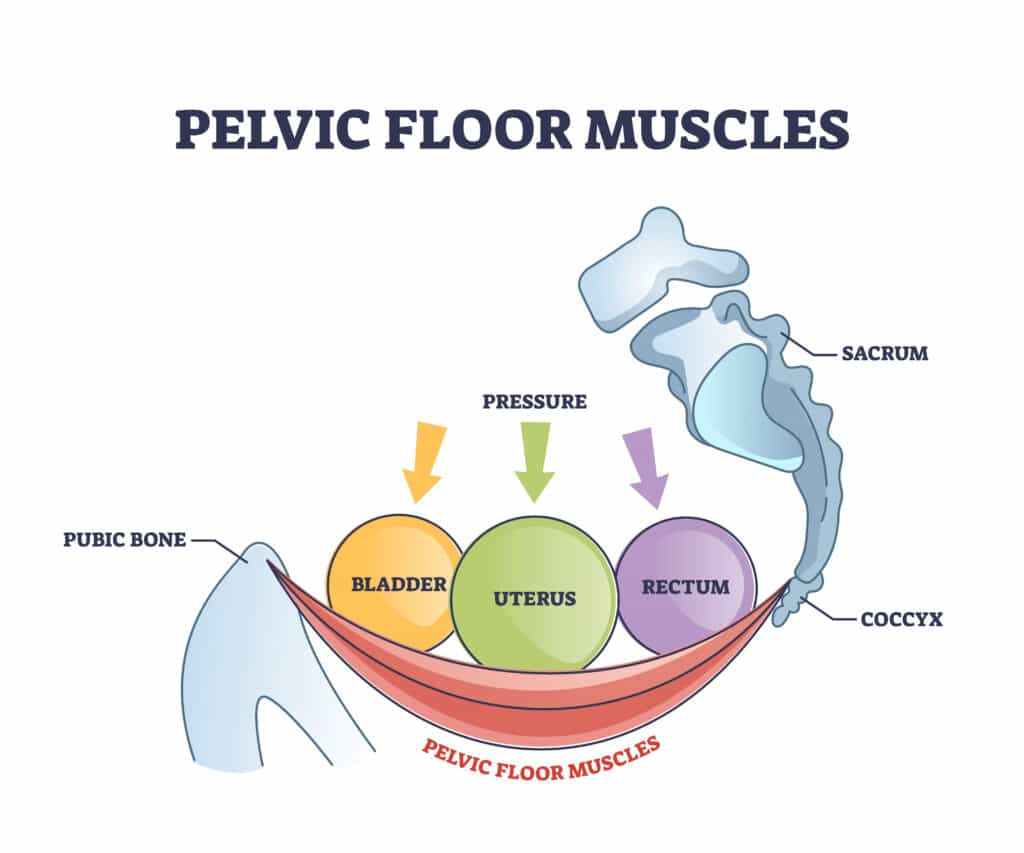
To understand why this happens, it’s helpful to know that the urethra is normally held in place by ligaments, muscles, and tissue. As illustrated in the graphic above, these structures provide support and keep everything in its proper position.
When these supportive elements weaken, the urethra can slip out of place, leading to various symptoms and complications.
In women, this might mean seeing or feeling a small bulge near the vaginal opening, experiencing discomfort, or noticing issues with urination. It might appear as a protrusion through the urethral opening, causing similar symptoms in men.
Recognizing these signs early and seeking medical advice can help manage the condition effectively and prevent further complications.
Urethral Prolapse Classification and Severity

Urethral prolapse is classified based on the degree of tissue protrusion and the severity of symptoms, ranging from mild to severe.1
Mild Urethral Prolapse
Mild urethral prolapse means the tissue only protrudes slightly beyond the urethral opening. Typically, this appears as a small, soft bulge less than 1 cm in diameter.
People with mild cases might not notice symptoms or feel discomfort or irritation. Minor bleeding might also occur.
Simple home care can often help mild cases. However, it is always important to seek professional advice before attempting to treat any condition at home.
Treatment usually involves simple measures such as warm water baths, applying special creams (like estrogen cream), and maintaining good hygiene. These conservative treatments are often sufficient to manage mild cases.
Moderate Urethral Prolapse
Moderate urethral prolapse involves a more noticeable protrusion, usually ranging from 1 cm to 2 cm in diameter. This level of prolapse can cause more discomfort, irritation, heavier bleeding, and problems with urination, such as pain or needing to go more often.
In addition to the basic treatments for mild cases, doctors might prescribe hormone therapy and monitor the condition closely.
Sometimes, a pessary—a small support device—may be used to support the prolapsed tissue and alleviate symptoms. We’ll discuss the role of pessaries in more detail later.
Severe Urethral Prolapse
Severe urethral prolapse is characterized by significant tissue protrusion, often more than 2 cm in diameter, extending well beyond the urethral opening. This can lead to considerable discomfort, continuous bleeding, difficulty urinating, or even infections.
Severe cases typically require more intensive treatments and often necessitate surgical intervention.
Surgical procedures might include the excision of the prolapsed tissue and repair of the urethral area to restore normal anatomy, especially if other treatments are ineffective or if complications arise.
Understanding the severity of urethral prolapse helps in determining the appropriate treatment approach. Early diagnosis and proper management are crucial in preventing complications and ensuring effective treatment.
If you notice any symptoms of urethral prolapse, consult a healthcare professional for an accurate diagnosis and personalized treatment plan.
Causes and Risk Factors for Urethral Prolapse

Understanding the causes and risk factors of urethral prolapse is important for finding the best ways to prevent and treat it.
Advanced Age
As people age, especially women after menopause, their estrogen levels naturally decline. Estrogen is essential for keeping muscles strong, including those in the pelvic floor.
When estrogen levels drop, these muscles and ligaments become weaker, making it easier for the urethra to move out of its normal position. Aging also weakens tissues overall, which increases the risk.
Pregnancy and Childbirth
Pregnancy and childbirth put a lot of stress on the pelvic floor muscles. During pregnancy, the baby’s weight adds pressure to the pelvic area.
Childbirth, especially vaginal delivery, involves a lot of force and stretching of the pelvic floor muscles. This can cause tears or overstretching, weakening the support for the urethra. The damage from childbirth might not show up right away but can lead to prolapse years later.1
Overweight, Strain or Pressure on Tissues
Increased pressure on the abdomen can also lead to urethral prolapse. Regularly lifting heavy objects, being overweight (obesity), chronic coughing, and straining during bowel movements all add pressure to the abdomen.
Over time, this pressure weakens the pelvic floor muscles, making them less able to support the urethra.
Previous Medical Treatments
Another big risk factor is previous pelvic surgery or trauma. People who have had surgery for pelvic organ prolapse or other related conditions might have weaker pelvic floor muscles.
While these surgeries are often necessary, they can sometimes weaken the pelvic support structures, making future prolapses more likely. Each additional surgery can make the problem worse, so it’s important to manage the condition and do strengthening exercises.
Regardless of whether it related to any of the above conditions, urethral prolapse often happens due to the weakening of the pelvic floor muscles and tissues supporting the urethra. A physical therapist specializing in pelvic floor health will often provide valuable insight to help you recover.
Symptoms of Urethral Prolapse
Urethral prolapse can present with symptoms ranging from mild to severe and can significantly impact daily activities and overall quality of life. Early recognition of these symptoms is crucial for effective management and treatment.
Early Signs and Irritation
One of the earliest signs of urethral prolapse is irritation in the vaginal or vulvar area or, in men, at the end of the penis.
This discomfort happens because the prolapsed urethra rubs against the surrounding tissue, causing redness, soreness, and a persistent itch that doesn’t go away with typical treatments for common infections.
Urinary and Bowel Issues
Urethral prolapse often leads to urinary problems, including blood in the urine and stress incontinence, which is leakage of urine during activities that increase abdominal pressure, like coughing, sneezing, or lifting heavy objects.
Some people may have trouble emptying their bladder completely, leading to frequent urination or a feeling that they haven’t fully emptied their bladder. These symptoms can cause embarrassment and anxiety, affecting social interactions and mental health.
Although less common, some individuals with urethral prolapse may also experience bowel problems, such as constipation or a sensation of rectal fullness. The prolapse can put pressure on the rectum, complicating bowel movements and causing straining, which can make the condition worse.
Pelvic Pressure and Pain
Many individuals report a constant feeling of fullness or pressure in the pelvic and genital areas. This sensation is often compared to feeling like you’re carrying a small ball inside the pelvis.
The pressure can become more noticeable during physical activities such as walking, exercising, or standing for long periods.
Chronic pelvic pain or aching discomfort is another common symptom. This pain varies in intensity and is usually located in the lower abdomen or pelvic region. It often gets worse towards the end of the day, after prolonged activity, or during menstruation.
Additionally, painful intercourse (dyspareunia) is associated with urethral prolapse. The displaced urethra and vaginal irritation can make sexual activity uncomfortable or painful, leading to decreased sexual desire and intimacy issues within relationships.1
Visible Protrusion
In more advanced cases, a visible bulge of tissue may protrude from the vaginal, penile, or urethral opening.
This can be alarming and uncomfortable, making it difficult to sit or walk. The protruding tissue can be sensitive to touch and easily irritated by clothing, leading to further discomfort.
Frequent UTIs
Structural changes in the pelvic area due to urethral prolapse can lead to recurrent urinary tract infections (UTIs).
The altered position of the urethra can make it easier for bacteria to enter the urinary tract, leading to frequent infections that need medical treatment.
If you’re encountering any of these symptoms, schedule an appointment with your doctor, as many of these issues can also indicate other conditions as well.
What to Expect at Physical Therapy for Urethral Prolapse
Pelvic health physical therapy (PT) is essential for effectively managing urethral prolapse.
A PT will first conduct thorough assessments to evaluate the pelvic floor muscles’ strength, coordination, and overall function. This evaluation helps identify each patient’s specific issues and needs.
Based on these assessments, therapists design individualized exercise programs tailored to each patient’s unique condition and capabilities, aiming to strengthen the pelvic floor and support proper muscle function.
Common Examinations, Manual Therapy & Guidance
Although it is not commonly a preferred procedure, internal exams and palpation may be necessary for issues like these.
Internal examination may feel invasive or even embarrassing for many patients, but remember that this is the professional clinical role of pelvic floor therapists. Getting comfortable with your therapist can help ensure that you feel safe for this or any other pelvic exam.
Manual therapy techniques also improve muscle function and alleviate discomfort through hands-on manipulation.
Education is another crucial aspect of pelvic health physical therapy. Patients learn about their condition, how to perform exercises correctly, and lifestyle modifications that can help manage symptoms.
Therapists provide ongoing support and motivation throughout the treatment process, encouraging adherence to the prescribed program and helping patients effectively achieve their health goals.
Physical Therapy Exercises for Urethral Prolapse
As a physical therapist, I focus on noninvasive, exercise-based interventions as a first line of defense to conservatively manage urethral prolapse symptoms and improve pelvic health.
Exercises can include those that strengthen the pelvic floor and deep abdominal muscles and improve muscle coordination and control.2,3
While the exercises below have helped many of my patients recover, it is important to get screened for your own needs, as other screening techniques may be needed for a proper assessment of your condition.
Kegel Exercises: The Fundamental Pelvic Floor Program
Kegel exercises are fundamental for strengthening the pelvic floor muscles, which support the bladder, uterus, and bowels.
Here’s how to perform them effectively:
- Identify the Muscles: Locate the correct muscles by imagining stopping the flow of urine mid-stream. The muscles you use to do this are your pelvic floor muscles.
- Contract: Once you have identified the correct muscles, tighten them for 3 to 5 seconds. Do not tighten your abdomen, thighs, or buttocks—focus solely on the pelvic floor muscles.
- Relax: Release the contraction and relax your muscles completely for 5 to 10 seconds. Giving your muscles enough time to rest between contractions is crucial for effective strengthening.
- Repeat: Aim to perform 10 to 15 repetitions in one session. For optimal results, try to complete three sessions a day.
Regular practice can significantly improve muscle tone, enhance bladder control, and reduce symptoms of urethral prolapse.
Consistency is key. Try to integrate Kegel exercises into your daily routine, such as while brushing your teeth, watching TV, or sitting at your desk.
Remember to breathe normally and ensure you are in a comfortable position to maximize effectiveness.
Core Strengthening for Urethral Prolapse
Strengthening the core muscles, including the transverse abdominis, can provide additional support to the pelvic floor. The transverse abdominis (TA) is the deepest layer of abdominal muscles and plays a crucial role in stabilizing the core and supporting the pelvic organs.
The TA functions like a girdle around your midsection and is closely related to and coordinated with your pelvic floor muscles.
For this reason, strengthening this muscle can help lessen symptoms associated with urethral prolapse by providing better support to the pelvic floor. Some effective exercises to target and strengthen the TA include:
Basic Exercises
Abdominal Bracing
- Lie on your back with your knees bent and feet flat on the floor.
- Place your hands on your lower abdomen. Take a deep breath, and as you exhale, draw your belly button towards your spine without moving your pelvis or ribs. Imagine tightening a corset around your waist.
- Maintain this contraction for 5 to 10 seconds while breathing normally. Relax and repeat.
Bracing Heel Slide
- Place your hands on your lower abdomen. Take a deep breath, and as you exhale, draw your belly button towards your spine without moving your pelvis or ribs. Imagine tightening a corset around your waist.
- While maintaining that engagement, slowly slide your heel toward your butt.
- Maintain this contraction for 5 to 10 seconds while breathing normally, then slide your heel back to the straight leg position.
- Relax and repeat.
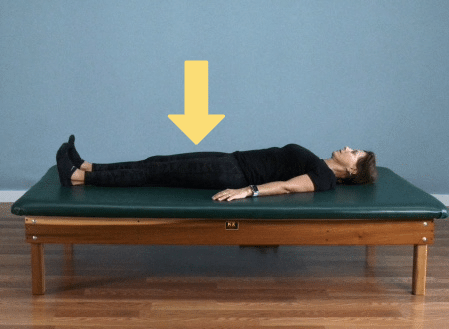
Supine Head Lift (mini curl-up)
- Lying on your back, brace your core muscles just as you have in the previous exercises.
- Next, lengthen the back of your neck and tuck your chin. This will feel like you are trying to intentionally create a “double chin”
- With you neck in this lengthened position, keep your core braced as you lift the back of your head off the surface you are lying on, as if trying to look at your belly.
- Hold this position for three to five seconds, rest and repeat for 10-12 repetitions.
Advanced Exercises
Dead Bug Level 2
- Lie on your back with your arms extended towards the ceiling and your knees bent at a 90-degree angle above your hips.
- Engage your TA by drawing your belly button towards your spine.
- Slowly lower your right arm and left leg towards the floor simultaneously, keeping your lower back pressed against the floor.
- Bring your arm and leg back to the starting position and switch sides.
- Perform 10 to 12 repetitions on each side.
Plank
- Start on your hands and knees.
- Lower your forearms to the floor with your elbows aligned under your shoulders.
- Step your feet back, coming into a plank position with your body in a straight line from head to heels.
- Engage your TA by drawing your belly button towards your spine.
- Maintain this position for 20 to 60 seconds, focusing on keeping your core tight and your body straight.
- Lower your knees to the floor and rest. Repeat 2 to 3 times.
Note: Although these exercises can be practiced at home, it’s always best to consult your PT before attempting any exercises that might inadvertently worsen your condition.
While practicing the basic exercises at home may be safe, be sure to schedule an appointment before doing the more advanced exercises.
Sarah’s Success Story: Overcoming Urethral Prolapse Without Surgery
I once worked with a patient named Sarah, a 58-year-old woman who experienced discomfort and frequent urination due to mild urethral prolapse.
She was anxious about the potential for surgery but was relieved to learn about non-invasive options. We started with a tailored exercise program that included Kegel exercises and core strengthening routines.
Over a few months, Sarah noticed significant improvements in her symptoms. She felt more in control of her bladder, experienced less discomfort, and regained confidence in her daily activities.
By sticking to the exercise regimen and making a few lifestyle adjustments, Sarah was able to manage her condition effectively without the need for surgical intervention.
Biofeedback and Other Treatment Options for Urethral Prolapse

When managing urethral prolapse, it’s important to explore a range of treatment options, from non-invasive techniques to surgical interventions.
This section covers biofeedback, a key tool for enhancing pelvic floor muscle control, and other approaches, such as pessaries and hormone treatments, that can offer significant relief.
Biofeedback for Pelvic Floor Muscle Training
Biofeedback is a technique that helps people become more aware of their pelvic floor muscles and improve control over them.
During a biofeedback session, sensors are placed either internally (vaginal or rectal) or externally (surface electrodes) to measure muscle activity. The data collected by these sensors is then shown in real time on a screen or through sounds.
This immediate feedback allows patients to see how well they contract and relax their muscles, helping them adjust their efforts and perform exercises more accurately.4
When is Biofeedback Used?
This technique is especially useful for improving muscle coordination and strength. By providing visual or auditory cues, biofeedback helps individuals learn to isolate and engage their pelvic floor muscles correctly.
It is often used to treat conditions like urinary incontinence, pelvic prolapse, and chronic pelvic pain. Biofeedback also allows for personalized exercise programs and tracks progress objectively, which can motivate patients and improve adherence to their rehabilitation efforts.
Non-Surgical Treatment Options
Several treatment options are available for advanced cases of urethral prolapse to address the condition and provide relief. One common non-invasive solution is the use of pessaries.
A pessary is a silicone device inserted into the vaginal canal to help maintain the structural integrity of the vaginal walls.
Pessaries come in various sizes and shapes to fit individual needs and are often recommended before considering surgical interventions. They offer significant symptom relief by providing support to the pelvic organs.1
Topical hormones, specifically estrogen creams, are another treatment option. These creams are applied directly to the affected area to help strengthen weakened tissues by replenishing hormone levels that may have declined, particularly in postmenopausal individuals.
Surgical Treatment Options
When non-surgical treatments are insufficient, surgical treatments may be necessary.
Procedures such as anterior vaginal wall repair are used to surgically reinforce the pelvic support structures, addressing the prolapse more permanently.
Surgery is typically considered when other treatments fail to provide adequate relief or if the prolapse is severe.
By understanding and utilizing these various treatment options, patients can effectively manage the symptoms of urethral prolapse and improve their quality of life.
Long-Term Management of Urethral Prolapse

While mild urethral prolapse might not cause symptoms, advanced cases can significantly impact daily life.
Physical therapy offers numerous non-invasive treatment options to manage symptoms and improve quality of life. By working closely with a pelvic health physical therapist, individuals can achieve long-term relief and better manage their condition.
Patients can take proactive steps toward managing this condition by understanding urethral prolapse, its symptoms, and treatment options.
Regular consultations with healthcare professionals and adherence to recommended therapies can ensure the best outcomes and help maintain a higher quality of life.
Taking charge of your pelvic health with the right information and support can make a significant difference in managing urethral prolapse.
Key Takeaways
- Urethral prolapse is when the urethra slips from its normal position, often pushing into the vaginal canal or protruding through the urethral opening.
- It is more common in females but can also occur in men.
- Early signs include irritation, discomfort, and urinary issues.
- The condition is classified as mild, moderate, or severe based on tissue protrusion and symptoms.
- Causes include weakening of pelvic floor muscles, aging, menopause, pregnancy, childbirth, increased abdominal pressure, and previous pelvic surgeries.
- Symptoms range from mild irritation to significant discomfort, frequent urinary tract infections, and visible tissue protrusion.
- Physical therapy is a crucial intervention, focusing on strengthening pelvic floor muscles through tailored exercise programs.
- Kegel exercises and core strengthening exercises, like abdominal bracing and planks, are effective for managing symptoms.
- Biofeedback helps improve pelvic floor muscle control and is useful for urinary incontinence and chronic pelvic pain.
- Non-surgical treatments include pessaries and estrogen creams, while severe cases may require surgical interventions.
- Early diagnosis and proper management can prevent complications and improve the quality of life.
- Regular consultations with healthcare professionals and adherence to recommended therapies are essential for effective management.
FAQs
What is urethral prolapse, and how is it classified?
Urethral prolapse occurs when the urethra slips from its normal position, often pushing into the vaginal canal or protruding through the urethral opening. It is classified into mild, moderate, or severe based on the degree of tissue protrusion and associated symptoms.
What causes urethral prolapse, and who is at risk?
The weakening of pelvic floor muscles often causes urethral prolapse due to factors like aging, menopause, pregnancy, childbirth, increased abdominal pressure, and previous pelvic surgeries. Women, especially postmenopausal women, are at higher risk, though the condition can also occur in men.
What are the common symptoms of urethral prolapse?
Common symptoms of urethral prolapse include irritation or discomfort in the vaginal or urethral area, urinary issues like incontinence or frequent urination, a feeling of pelvic pressure, visible tissue protrusion, and in more advanced cases, recurrent urinary tract infections (UTIs).
How can physical therapy help manage urethral prolapse?
Physical therapy is essential in managing urethral prolapse by focusing on strengthening the pelvic floor muscles. Tailored exercise programs, such as Kegel exercises and core strengthening, help improve muscle function and reduce symptoms, often preventing the need for surgical intervention.
What are the non-surgical treatment options for urethral prolapse?
Non-surgical treatment options for urethral prolapse include the use of pessaries, which are silicone devices inserted into the vaginal canal to support the pelvic organs, and topical estrogen creams to strengthen weakened tissues. Biofeedback is also used to improve pelvic floor muscle control.
When is surgery necessary for treating urethral prolapse?
Surgery is typically considered when non-surgical treatments fail to provide adequate relief or if the prolapse is severe. Surgical options, such as anterior vaginal wall repair, are used to reinforce pelvic support structures and address the prolapse more permanently.
References
- Fornari, Alexandre et al. “Urethral Prolapse: A Case Series and Literature Review.” Journal of Obstetrics and Gynaecology of India vol. 70,2 (2020): 158-162. doi:10.1007/s13224-019-01288-2
- Knorst, Mara R et al. “Physical therapy intervention in women with urinary incontinence associated with pelvic organ prolapse.” Revista brasileira de fisioterapia (Sao Carlos (Sao Paulo, Brazil)) vol. 16,2 (2012): 102-7.
- Bø, Kari. “Pelvic floor muscle training is effective in treatment of female stress urinary incontinence, but how does it work?.” International urogynecology journal and pelvic floor dysfunction vol. 15,2 (2004): 76-84. doi:10.1007/s00192-004-1125-0
- Therapeutic efficacy of biofeedback pelvic floor muscle exercise in women with dysfunctional voiding | Scientific Reports (nature.com)





