Regardless of your age, its very likely that you know someone who is dealing with the effects of Parkinson’s Disease.
Parkinson’s disease (PD) is a progressive brain disorder caused by a degeneration of nerve cells in an area of the brain that controls many aspects of movement, including speech. People with PD move through stages of severity. Resulting movement disorders through these stages range from mild tremors to severe disruption of the nervous system.
According to the Parkinson’s Foundation, Parkinson’s Disease is the second most common neurodegenerative disease in the United States, with Alzheimer’s being the first.
Rehabilitation professionals—including physical therapists, can help guide you through a curated treatment plan after a diagnosis. A targeted, therapist-guided exercise program can improve functionality and quality of life.
Whether you’re concerned about risk factors or are actively dealing with Parkinson’s or other neurodegenerative diseases, understanding what Parkinson’s is, how it is treated, and what to expect is critical to getting ahead of this disease. We’ll also share how exercise and movement interventions are the only current methods to slow the progress of Parkinson’s Disease.
What Is Parkinson’s Disease?
PD affects the central nervous system, resulting in motor symptoms like tremors, rigidity, and worsening balance. The progression of this disease can result in disability and the need for a caregiver.
Over one million people in the United States are living with Parkinson’s (PD)—more than multiple sclerosis (MS), muscular dystrophy (MD), and amyotrophic lateral sclerosis (ALS) combined.
Men are at a higher risk for developing Parkinson’s disease at about a 1.5 to 1 ratio.1
What Causes Parkinson’s?
The onset of Parkinson’s is usually sporadic or idiopathic, meaning it develops without a known cause. While no specific cause has been identified, genetic and environmental factors are assumed to be involved.
Environmental toxins, drugs (antipsychotics or antiemetics), or certain infections may play a role in the development of PD. Only 5-10% of Parkinson’s cases are related to genetics.
Tiny clusters of cells called Lewy bodies are present in the brain of people with Parkinson’s and another related neurodegenerative disease called Lewy Body Dementia. These mysterious cells hold potential clues to the causes of Parkinson’s disease and are the focus of significant research.
Is Parkinson’s an autoimmune disease?
An autoimmune disease occurs when overactive immune cells mistakenly target the body’s healthy functional tissues. Autoimmune conditions can occur in most of the body’s systems and tissues.
There is some recent research indicating that Parkinson’s may at least be, in part, due to autoimmunity. Still, it has not yet been classified as an autoimmune disease.2
The Anatomy & Physiology of Parkinson’s
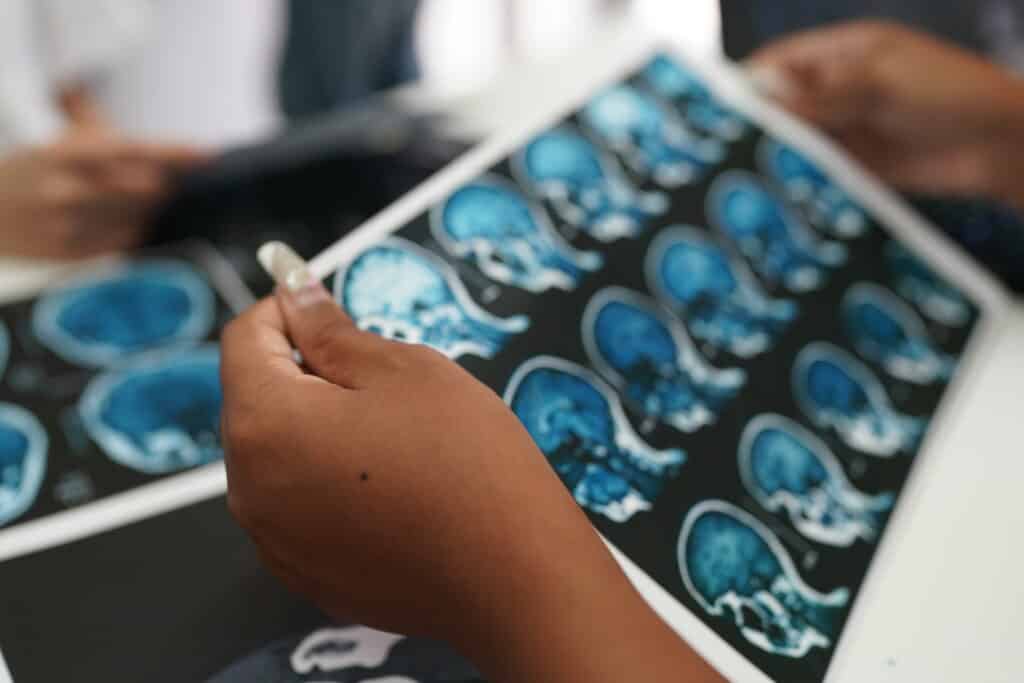
The area of the brain that experiences the most degeneration during Parkinson’s disease is called the substantia nigra. This area of the brain handles the production of dopamine, a neurotransmitter that aids in controlling movement, among other things.
With Parkinson’s, dopamine production slowly degenerates, impacting how the brain sends signals to the rest of your body. This chemical imbalance can result in both physical (motor) and cognitive symptoms, affecting both the central nervous system (the brain and spinal cord) and the peripheral nervous system (arms, legs, and torso).3
Symptoms
Motor Symptoms
The various motor symptoms are hallmarks of Parkinson’s disease. Common symptoms are categorized as “parkinsonism.”
Parkinsonism includes:
- Bradykinesia, or slower-than-usual movement
- Cogwheel rigidity or muscle stiffness accompanied by tremors.
- Resting tremors
- Micrographia, or handwriting that gets smaller as you write
- Hypomimia, or dulling of facial expressions.
Parkinson’s gait or Parkinson’s walk tends to become noticeable when walking.
This simplified symptom may include decreased arm swing, shuffling steps, freezing gait, frequent falls, instability, and hunched posture. Similarly, getting up from a chair, out of a car, or standing up from bed may become increasingly difficult over time.4
Parkinson’s symptoms almost always start on one side of the body. They do not begin to occur on the other side until later in the disease. This is one of the significant early determinants of PD compared to similar neurodegenerative disorders.
Non-Motor Symptoms
Some of the non-motor features of Parkinson’s that you might experience include memory impairments, a decreased sense of smell, internal tremors, fatigue, orthostatic hypotension (low blood pressure leading to fainting), urinary urgency, constipation, swallowing problems, or sleep issues.
These are often less recognized than the more prominent and noticeable motor symptoms but can be just as debilitating for many people with PD.
Other symptoms of late-stage Parkinson’s include depression, anxiety, hallucinations, or psychosis.
Related Articles
- The Five Stages of Parkinson’s Disease
- Parkinson’s Exercise Programs
- How a Vibrating Parkinson’s Glove Could Change Future Treatment
- The Importance of Physical Therapy for Parkinson’s Disease
- PWR Moves: Exercises for Parkinson’s Disease
Progression
There are five commonly known stages of Parkinson’s disease, which outline the typical progression of motor symptoms. Symptoms typically start with a unilateral tremor and can progress over the years.
In the later stages of Parkinson’s, people tend to rely increasingly on assistive devices like walkers, wheelchairs, and even specialized cutlery while eating. You may also later require caregiver support and experience serious cognitive impairments.
The Essential Neurology of Parkinson’s Disease
Diving further into the neurological inner workings of Parkinson’s, we uncover the intricate balance of brain chemistry, genetic threads, and environmental cues that shape this condition.
With an eye on the latest research, let’s explore the pivotal recent areas of study that offer new hope and understanding about managing and potentially transforming the future of PD treatment and research.
Dopamine and the Brain
In Parkinson’s, the decline in dopamine-producing neurons, particularly in a brain area called the substantia nigra, disrupts the body’s movement control. This deficiency manifests in tremors, stiffness, and slowness.
Today’s treatments aim to alleviate these symptoms by supplementing dopamine or mimicking its action. Research is now advancing towards neuroprotective strategies and gene therapy, with the hope of preserving these crucial neurons and decelerating the disease’s progression.
These new methods offer a glimmer of hope for more effective treatments on the horizon.
The Role of Lewy Bodies
Lewy bodies, identified as abnormal protein accumulations, play a significant role in Parkinson’s pathology. These proteins, primarily alpha-synuclein, contribute to the breakdown of neural communication and function, leading to Parkinson’s symptoms.
Recent research delves into how Lewy bodies form and their precise impact, aiming to uncover treatments that can target these proteins directly.
This understanding is pivotal in developing therapies beyond symptom management to fundamentally alter the disease’s trajectory.
Genetic Factors in Parkinson’s
About 10% of Parkinson’s cases are linked to genetic factors, with mutations in genes such as LRRK2 and SNCA shedding light on the disease’s hereditary aspects. This genetic understanding clarifies risk factors and steers research toward personalized treatments.
Advances in genetic technology offer hope for interventions that could one day prevent or significantly slow the progression of Parkinson’s in individuals with a genetic predisposition, marking a promising frontier in the battle against the disease.
Environmental Influences on Parkinson’s
The role of environmental factors in Parkinson’s underscores the disease’s complexity.
Exposures to certain pesticides and heavy metals have been correlated with an increased risk of developing Parkinson’s, highlighting the interaction between genetics and environmental triggers.
Identifying these toxins and understanding their mechanisms are critical for developing preventive strategies and informing safer environmental practices, potentially reducing Parkinson’s prevalence.
Inflammation and Cell Stress
Emerging evidence points to inflammation and oxidative stress as key players in Parkinson’s progression, contributing to neuronal damage.
Research into these areas explores potential treatments to mitigate these processes, offering a promising avenue for slowing disease progression.
By targeting these underlying mechanisms, scientists aim to develop therapies that manage symptoms and address the root causes of neuronal damage in Parkinson’s.
The Gut-Brain Connection: A Novel Perspective on Parkinson’s
Recent studies highlight the gut-brain axis’s role in Parkinson’s, suggesting that gut health may directly influence brain health and disease development.
This insight opens up new research directions, including how dietary changes and probiotics could support brain health and potentially slow Parkinson’s progression.
Understanding this connection could revolutionize treatment approaches, emphasizing the importance of holistic health in managing and potentially preventing Parkinson’s.
Parkinson’s and Other Neurological Conditions
Parkinson’s is similar, but not the same, as many other neurodegenerative diseases, including multiple sclerosis, amyotrophic lateral sclerosis, and Lewy body dementia.
Multiple sclerosis is an autoimmune condition in which the immune system attacks the myelin surrounding nerve fibers throughout the central nervous system, resulting in various nerve problems.
MS is often diagnosed between the ages of twenty and forty, while Parkinson’s is typically diagnosed at sixty and up. While PD is progressive, MS can be more erratic and often comes in “attacks,” leading to more steady degeneration.
Amyotrophic lateral sclerosis, widely known as Lou Gehrig’s disease, causes muscle weakness and atrophy alongside similar symptoms to those that people with Parkinson’s might encounter.
ALS patients struggle with specific motor patterns like chewing, talking, and gait. There is no known cure, nor is there a treatment that slows the progression of ALS.
Treatment Options

Unfortunately, there is currently no cure for Parkinson’s. Still, medications and other treatments can help with symptom management as the disease progresses.
Exercise and physical therapy can slow PD symptom progression. Various exercises can help to manage Parkinson’s rigidity, while others can improve Parkinson’s gait and other movement problems.
Medication for Parkinson’s Disease
Many medications can ease your Parkinson’s symptoms.
Levodopa, a drug that converts into dopamine, is helpful in early to moderate PD but becomes less effective in later stages of the disease progression.
Other medications directly target motor or non-motor symptoms. They may include drugs to counter or manage secondary psychological symptoms like depression or psychosis.5
Role of Exercise & Neuroplasticity
The only thing that can truly slow down the disease is exercise.
Exercise can increase dopamine release in some areas of the brain. It can also prevent excessive dopamine absorption, making it available for use. People with a history of exercise are less likely to develop Parkinson’s in the first place.
Because of its many benefits, the CDC recommends that older adults participate in 150 minutes per week of exercise as a combination of cardiovascular and strength training.
Regular exercise is associated with better quality of life, mobility, physical function, and cognition for all older adults. Still, it is specifically beneficial to those with Parkinson’s.4
Physical Therapy
Exercise has been proven to have neuroprotective and disease-modifying capabilities for Parkinson’s. A targeted and supervised medical exercise program can be integral for disease management.
An assessment by a physical therapist might include testing for balance, cognition, strength, posture, and endurance. Treatment goals for PD focus on slowing the progression of the disease and the progression of disability that comes with it.
Critical components of a Parkinson’s exercise program should include cardiovascular exercise and task-specific strength and balance training to maintain normal function for as long as possible.
Ideally, exercise allows independence for all your desired activities. It maintains or improves functional abilities to enhance your quality of life. Additionally, exercise can help to prevent falls and improve stability.
Ongoing Research & Other Promising Treatments
When disability becomes severe, surgical treatment options can help.
For example, deep brain stimulation inserts electrodes into the brain to stimulate dysfunctional areas of brain cells or regions.
Research is investigating the efficacy of other treatment methods, including injections to improve dopamine production and studies about how gene therapy might impact the development of PD. 3
Living with Parkinson’s

Being diagnosed at early stages can result in more effective treatments and a better quality of life for the duration of the disease progression.
Parkinson’s is a challenging disease for the person diagnosed, loved ones, and caregivers alike. Joining a Parkinson’s support group can help improve the physical and psychological health of everyone affected by a diagnosis.
It can also be helpful to explore community resources, such as fitness groups and exercise classes for those with Parkinson’s.
Please refer to this helpful article for more information about managing Parkinson’s disease with physical therapy and exercise.
Key Takeaways
- Parkinson’s Disease is a progressive disorder affecting movement and speech.
- It’s the second most prevalent neurodegenerative disease in the U.S.
- Symptoms range from tremors to severe motor impairment.
- Men are more likely to develop PD than women.
- The exact cause of PD is unknown, but genetics and environment may contribute.
- Dopamine-producing brain cells are lost in PD.
- PD’s symptoms include both motor issues like stiffness and non-motor problems like memory loss.
- The disease usually starts on one side of the body and gets worse over time.
- No cure exists for PD, but medications and physical therapy help manage symptoms.
- Regular exercise can slow disease progression and improve life quality.
- Deep brain stimulation surgery is an option for advanced PD.
- Early detection of PD can lead to better management of the condition.
- Support systems are important for those affected by PD.
FAQs
How can physical therapy benefit seniors with Parkinson’s?
Physical therapy can provide numerous benefits for seniors with Parkinson’s Disease. It helps maintain and improve mobility, flexibility, and balance, which can reduce the risk of falls.
Physical therapy can also target specific symptoms of Parkinson’s, such as rigidity and bradykinesia (slowness of movement), helping seniors retain more of their functional independence for as long as possible.
Additionally, it can provide strategies to manage symptoms, adapt to changes in physical abilities, and maintain a higher quality of life.
What are the first signs of Parkinson’s disease?
The earliest indications of Parkinson’s disease often involve subtle but noticeable changes in movement. A tremor in one hand, particularly a “pill-rolling tremor” at rest, is a common early sign.
Others might experience stiffness or rigidity in the limbs and trunk, which does not subside with movement, or they may notice their movements becoming slower—a condition known as bradykinesia. Some individuals also encounter changes in posture and balance early on, and facial expressions may become less animated.
What treatments are available for Parkinson’s disease?
While there is no cure for Parkinson’s disease, various treatments can manage its symptoms. Medications, such as Levodopa and dopamine agonists, are often prescribed to increase or substitute for dopamine, a neurotransmitter that’s reduced in the brains of those with Parkinson’s.
Surgical interventions like deep brain stimulation (DBS) might be appropriate for some patients. Physical therapy, exercise, and lifestyle changes are crucial for managing symptoms and maintaining mobility and function.
Can physical therapy delay the progression of Parkinson’s in seniors?
While physical therapy cannot halt the progression of Parkinson’s Disease, which is a progressive neurological disorder, there is evidence to suggest that regular, targeted physical therapy exercises can help slow down the impairment of motor skills in seniors.
Through exercises designed to improve strength, flexibility, balance, and coordination, physical therapy can help seniors manage symptoms more effectively and maintain function, which might contribute to a perceived slowing of the disease’s progression in daily life activities. Regular exercise has been shown to have neuroprotective effects, meaning it can support the health of neurons and may potentially slow down the rate at which symptoms worsen.
Can Parkinson’s disease be cured or reversed?
Parkinson’s disease remains incurable, and its progression cannot be reversed. However, research is ongoing, and significant advancements have been made in managing symptoms and improving the quality of life for those affected.
Exercise and movement interventions are the only methods to slow the progress of Parkinson’s Disease at this time.
Current treatments focus on alleviating symptoms and slowing disease progression through medication, lifestyle modifications, and, in some cases, surgery. Research into gene therapy, neuroprotective agents, and other novel treatments continues to be a beacon of hope for potentially curative therapies in the future.
Resources
- Bloem, B. R., Okun, M. S., & Klein, C. (2021). Parkinson’s disease. The Lancet, 397(10291), 2284-2303.
- Jiang, T., Li, G., Xu, J., Gao, S., & Chen, X. (2018). The Challenge of the Pathogenesis of Parkinson’s Disease: Is Autoimmunity the Culprit?. Frontiers in immunology, 9, 2047. https://doi.org/10.3389/fimmu.2018.02047
- Lang, A. E., & Lozano, A. M. (1998). Parkinson’s disease. New England Journal of Medicine, 339(16), 1130-1143.
- Hayes, M. T. (2019). Parkinson’s disease and parkinsonism. The American journal of medicine, 132(7), 802-807.
- Connolly, B. S., & Lang, A. E. (2014). Pharmacological treatment of Parkinson disease: a review. Jama, 311(16), 1670-1683.
Armstrong MJ, Okun MS. Diagnosis and Treatment of Parkinson Disease: A Review. JAMA. 2020;323(6):548–560. doi:10.1001/jama.2019.22360
Parkinson’s Disease | PD | MedlinePlus
C. A. Davie, A review of Parkinson’s disease, British Medical Bulletin, Volume 86, Issue 1, June 2008, Pages 109–127, https://doi.org/10.1093/bmb/ldn013
Diagnosis and Treatment of Parkinson Disease: A Review | Movement Disorders | JAMA | JAMA Network
Schapira, Anthony (ed.), Parkinson’s Disease, Oxford Neurology Library (Oxford, 2010; online edn, Oxford Academic, 1 May 2011), https://doi.org/10.1093/med/9780199550630.001.0001, accessed 1 Feb. 2024.
Parashar, A., & Udayabanu, M. (2017). Gut microbiota: Implications in Parkinson’s disease. Parkinsonism & Related Disorders, 38, 1-7. https://doi.org/10.1016/j.parkreldis.2017.02.002
Kline, E. M., Houser, M. C., Herrick, M. K., Seibler, P., Klein, C., West, A., & Tansey, M. G. (2021). Genetic and Environmental Factors in Parkinson’s Disease Converge on Immune Function and Inflammation. Movement Disorders, 36(1), 25-36. https://doi.org/10.1002/mds.28411