Headaches, including migraines, tension, and cluster headaches, are a significant health issue globally, affecting nearly half of the adult population, as noted by the World Health Organization.
These conditions span all ages, races, and socioeconomic groups, often presenting a challenge in identifying their root causes.
This article will explore the various types of headaches, emphasizing a variety of headache treatment strategies. From lifestyle changes and traditional medical treatments to alternative therapies, this comprehensive guide will address your pain to improve your overall quality of life.
We’ll provide valuable insights into the different headache disorders and many ways to manage and reduce their impact. This straightforward resource is for anyone seeking to understand more about headaches and how to handle them effectively.
Common Types of Headaches and Their Causes
While there are many types of headaches, the most common primary headache disorders are tension headaches, migraines, cluster, and cervicogenic headaches. Let’s dig a little deeper into each kind for more detail.
Tension Headaches: The Everyday Headache
If you’ve ever felt a throbbing pain that feels like a tight band around your forehead or at the back of your head, you might have experienced a tension headache.
These headaches usually present as a dull, aching discomfort on both sides of your skull. If you’re an active older person, you might notice these headaches more often due to triggers such as stress, anxiety, fatigue, or muscle tension from physical activities.
Tension headaches typically start during the teenage years and may become more frequent as you age, particularly in your 40s. Women are more prone to tension headaches than men, so if you’re a woman, it’s crucial to be mindful of potential triggers.
Tension Headache Causes
Tension headaches, commonly caused by stress and anxiety, can also arise from musculoskeletal issues in the neck and upper back, often due to poor posture or repetitive strain. Sleep disturbances, including both lack of sleep and oversleeping, are another contributing factor. In today’s digital world, prolonged screen use leading to eyestrain frequently triggers these headaches.
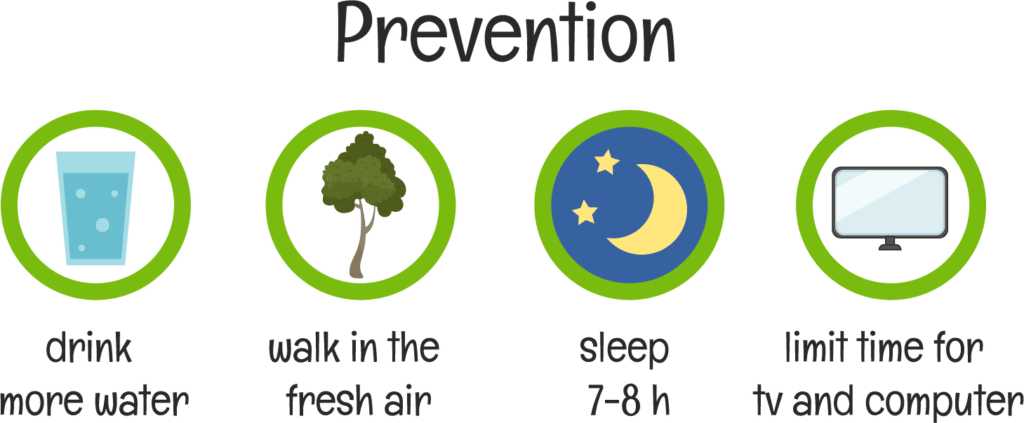
Additionally, dietary habits such as caffeine withdrawal, dehydration, skipping meals, or alcohol intake, as well as environmental factors like bright lights, loud noises, and strong odors, can also lead to tension headaches. Adopting a healthy lifestyle, managing stress effectively, and ensuring an ergonomic work environment can help mitigate these triggers.
Migraines: More Than Just a Headache
Migraine headaches are a more severe form of primary headache disorder. If you’ve ever experienced a migraine, you’ll know it’s not just a headache. Migraines often come with intense, throbbing pain typically located on one side of the head. Other symptoms like nausea, vomiting, and sensitivity to light and sound can also accompany them.
Causes of Migraine
Migraines are believed to be caused by changes in brain chemicals, including serotonin. Like tension headaches, they can be triggered by stress, anxiety, fatigue, and hormonal differences, especially in women.
Migraines often begin during puberty and tend to become more frequent between the ages of 35 to 45. Women are more prone to experiencing migraines compared to men, a difference that hormonal changes may influence. These hormonal fluctuations, particularly those occurring just before or after menstruation, are known to trigger migraines in women.
Additionally, genetics play a role in migraine susceptibility; individuals with a family history of migraines have an increased risk of developing them. This combination of age, gender, hormonal factors, and genetic predisposition outlines the typical profile of migraine occurrence and frequency.
Common Triggers for Migraine
Migraines are more complex, and their exact cause isn’t fully understood. However, environmental and genetic factors play a significant role. Changes in the brainstem and its interaction with the trigeminal nerve, a major pain pathway, may be involved.
Additionally, imbalances in brain chemicals, including serotonin, which helps regulate pain in your nervous system, and calcitonin gene-related peptides, which are released during a migraine, may also contribute to the occurrence of migraines.
Symptoms of Migraine Attacks: What to Look Out For
Migraine attacks, a specific type of headache, carry distinctive symptoms. These can include an increased sensitivity to light and sound, a throbbing or pulsing headache, and feelings of nausea.
Some people also experience what is known as auras – visual disturbances that can include seeing flashing lights, zigzag lines, or even temporary loss of vision.
Migraine Variants: Dizziness and Vestibular Migraines
In addition to the well-known symptoms, migraines can also cause dizziness. This symptom can be particularly disorienting and add to the discomfort experienced during a migraine attack.
A specific type of migraine known as a “vestibular migraine” can present with or without the typical headache. These migraines are characterized by vertigo, a form of dizziness where you or your surroundings feel like they are spinning.
Vestibular migraines may result in common migraine symptoms like nausea and light sensitivity, with the added challenge of balance disturbances due to vertigo.
Understanding these variants can help with proper diagnosis and treatment. The approach to managing vestibular migraines may differ from that of standard migraines.
Cluster Headaches
Cluster headaches, though rare, can be excruciating. They are characterized by severe, recurring pain on one side of the head and occur in cycles, with periods of no pain in between. These headaches often strike at night, and the pain can be so severe that it wakes people from sleep.
There is no known cure for cluster headaches. Still, treatments like triptans, ergotamines, corticosteroids, oxygen therapy, and nerve blocks can help manage symptoms.
Cluster headaches, while relatively rare and affecting only about 1 in 1000 people, typically begin in individuals in their early 20s, although they can occur at any age. Men are more frequently affected by these headaches compared to women.
A family history of cluster headaches also increases the likelihood of developing them, suggesting a genetic component. Additionally, most individuals who experience cluster headaches are smokers, and alcohol consumption has been identified as a potential trigger for an attack.
Cluster Headache Causes
The root cause of cluster headaches is also not completely clear. However, abnormalities in the hypothalamus, the part of the brain responsible for your body’s biological clock, could be involved.
This theory is based on the fact that cluster headaches often follow a seasonal pattern and occur regularly throughout 24-hour periods.
Cervicogenic Headaches: A Brief Overview
Cervicogenic headaches, a secondary type of headache, originate from neck disorders and often mimic the symptoms of migraines or tension headaches. These headaches typically start with neck discomfort and progress to one-sided head pain. The pain is usually constant, non-throbbing, and can worsen with neck movement.
The primary causes are cervical spine or neck muscle issues, often due to injury, arthritis, or prolonged strain. Diagnosis involves a neck examination and medical history review.
Treatment focuses on the underlying neck condition, with strategies like physical therapy, nerve blocks, or surgery in more severe cases. Addressing cervicogenic headaches is critical to holistic headache management and improving quality of life.
Factors Increasing the Risk of Headaches

Various factors can increase the likelihood of experiencing headaches. These include dehydration, hunger, over-use of medication, sleep problems, and mental health issues such as anxiety and depression.
Dehydration
Dehydration is a significant but often overlooked cause of headaches. Insufficient fluid intake can lower blood volume, reducing oxygen flow to the brain and triggering headaches. Symptoms can range from mild to severe, and staying hydrated is critical to prevention.
Hunger
Skipping meals or long gaps between eating can lead to headaches due to low blood sugar. This triggers the release of hormones like adrenaline, which can tighten blood vessels and cause headaches. Regular, balanced meals are essential to avoid these headaches.
Medication Overuse Headaches
Frequent use of headache medications, particularly pain relievers, can lead to medication-overuse headaches. This condition is characterized by chronic headaches that worsen as the medication effect wanes. Managing medication use and consulting healthcare providers is essential for avoiding this issue.
Sleep Deficiency
Inadequate sleep is a common trigger for headaches, particularly tension headaches and migraines. Insufficient rest can increase stress, disrupt hormonal balance, and elevate inflammation, contributing to headache onset and severity. People with erratic sleep patterns often report more frequent and intense headaches.
Enhancing Sleep for Headache Management
Improving sleep hygiene is vital for reducing headache occurrences. Essential practices include keeping a consistent sleep schedule, curating a comfortable sleeping environment, and avoiding caffeine and screens before bed.
For those with sleep-related headaches, a healthcare provider might suggest a sleep study to identify and treat any underlying sleep disorders. Better sleep not only helps diminish headache frequency but also improves overall health.
Mental Health and Its Impact on Headaches
Anxiety and depression are closely linked to headaches. Stress from these mental health issues can cause muscle tension and headaches. Moreover, depression can make individuals more sensitive to pain. Addressing mental health is crucial for headache management.
Standard Screens, Symptoms, and Headache Treatment Options

Understanding Imaging Studies: CT and MRI Scans
In some situations, your doctor might recommend imaging studies to get a more detailed look at what’s happening inside your body. Two standard imaging techniques are computed tomography (CT) and magnetic resonance imaging (MRI) scans.
A CT scan is a specialized X-ray that provides a detailed view of your body’s internal structures. It’s beneficial for diagnosing vascular headaches, which are headaches related to your body’s vascular or blood vessel system. This scan uses a contrasting dye to highlight the various structures in your body, making it easier for your doctor to spot abnormalities like tumors or hemorrhages.
On the other hand, MRI scans use a powerful magnetic field and radio waves to produce detailed images of your body’s internal structures. This can be particularly useful in diagnosing headaches related to neurological issues.
Nerve Blocks: A Diagnostic Tool
In cases where your doctor suspects that your headaches might be caused by irritation, inflammation, or damage to a nerve, a diagnostic nerve block might be recommended.
During this procedure, a combination of a steroid and anesthetic is injected into the area around the affected nerve. If you experience relief from your headache following this procedure, your discomfort is likely the result of a problem with a nerve.
Vision Checks and Migraine-Specific Diets
An often-overlooked aspect of headache management, particularly for migraines, is regular vision check-ups. Vision changes, however minor, can strain the eyes and contribute to the onset of headaches. Regular visits to an optometrist ensure that any vision changes are promptly addressed, potentially reducing the frequency of headaches related to eye strain.
In addition to eye care, dietary adjustments play a significant role in managing migraines. Certain foods are known to trigger migraines in susceptible individuals. A migraine-specific diet, which involves avoiding common triggers like aged cheeses, processed meats, chocolate, and foods containing MSG or artificial sweeteners, can be beneficial.
Keeping a food diary can help identify personal triggers and guide dietary choices. By combining regular vision care with mindful eating, individuals can proactively manage migraine symptoms and improve their overall quality of life.
Prescription or Over-the-Counter Medications
One commonly used method is over-the-counter pain relievers and anti-inflammatory medications. But medication for headaches comes with caveats.
For those experiencing severe or persistent headaches, more potent drugs such as triptans and opioids may be recommended. However, keep in mind that opioids should be used sparingly due to the risk of addiction.
Navigating Medication Overuse and Rebound Headaches
Monitoring medication overuse is critical in headache management, particularly concerning over-the-counter (OTC) pain relievers.
Using OTC medications like Aleve (naproxen), Ibuprofen, Advil, and similar drugs for headaches more than ten days a month can lead to a condition known as “rebound” headaches.
Rebound headaches occur when the medication, initially taken to relieve the headache, begins to cause headaches when used too frequently.
The body can become accustomed to the medication, and when it wears off, the headache returns, often more intensely. This can create a cycle where the individual takes more of the drug to relieve the new headache, perpetuating the problem.
To avoid rebound headaches, it’s essential to adhere to guidelines for OTC pain relievers and not exceed the recommended usage. For those experiencing frequent headaches, consulting with a healthcare provider is important to explore alternative treatment strategies. This may include prescription medications designed for frequent headaches, lifestyle changes, or other non-pharmacological approaches.
Breaking the cycle of medication overuse requires awareness and careful management but is a vital step in effective headache treatment and prevention.
Antiseizure Medications for Migraines
Antiseizure medications like topiramate, gabapentin, and carbamazepine are sometimes used to help older adults with migraines. Made initially for epilepsy, these drugs can also reduce how often and how severe migraines are. They work by calming brain nerves, which can prevent migraines.
It’s important for anyone using these medications to talk with their doctor about the best plan, considering side effects and other medicines they might be taking. Along with these drugs, simple lifestyle changes like managing stress, exercising, and eating well can also help control migraines. Patients should keep their doctor updated about their migraine patterns for the best results.
Cluster Headache Relief Options
For those suffering from cluster headaches, a few straightforward treatments can help. One effective method is inhaling oxygen through a mask, which can quickly reduce headache pain. Injectable triptans, another option, are medicines commonly used for migraine relief but also work for cluster headaches.
Additionally, octreotide, an injectable medication, and local anesthetics can be applied through a nasal spray to numb the area and lessen the pain. In more severe cases, dihydroergotamine, which is given as an injection, can also be effective.
Complementary and Alternative Therapies (CAM)
If you’re open to exploring alternative therapies, treatments like acupuncture, biofeedback, massage therapy, physical therapy, and chiropractic manipulation can provide symptom relief, particularly for tension headaches. These treatments aim to relieve muscle tension and improve joint function, which can significantly help manage headaches.
Headache disorders affect millions of active older adults, sometimes severely impacting their quality of life. However, with a mix of lifestyle changes, traditional medications, and alternative treatments, it’s possible to manage symptoms effectively.
Other Effective Lifestyle Modifications for Headache Treatment

You have the power to manage your headaches effectively through simple modifications like regular exercise, hydration, and eating right. Let’s explore some simple yet effective lifestyle changes you can make daily to eliminate headaches.
Regular Exercise
Physical activity is for more than just maintaining a healthy weight. It’s a natural remedy for headaches, too. Regular, low-impact exercises like walking, swimming, or cycling can help reduce the frequency and severity of your headaches.
Remember, it’s not about how strenuous your exercise is but how consistent you are with it. Frequent exercise is better than intense bouts, especially when dealing with headaches.
Maintain Good Posture
As we age, we can develop a tendency to slouch. This can strain your neck and shoulders unnecessarily, leading to tension headaches. Try to be mindful of your posture, especially when sitting for extended periods.
Take Regular Breaks
Take regular breaks if you find yourself in a position that strains your neck—like reading a book or looking at a computer screen. A simple stretch or a short walk can do wonders for your neck and head.
Coping with Stress
Stress is a common trigger for headaches. Learning effective stress management strategies, such as deep breathing, yoga, or even talking to a friend, can help you control your stress levels.
Regular Sleep
A good night’s sleep is essential for overall health and headache management. Establish a regular sleep schedule and create a peaceful sleep environment to ensure you get the rest you need.
Quit Smoking
Smoking can increase the likelihood of headaches. If you’re a smoker, consider seeking help to quit. It’s never too late to take this step towards better health.
Practice Relaxation Techniques
Techniques like mindfulness, meditation, and progressive muscle relaxation can help reduce headache frequency and intensity. These methods can help you relax and manage stress better.
Stay Hydrated
Dehydration can trigger headaches. Aim to drink at least eight glasses of water daily, even more if you’re physically active, or it’s a hot day.
Eating Healthy
A balanced diet rich in fruits, vegetables, lean proteins, and whole grains can help manage headaches. Avoid foods that trigger headaches, like chocolate, cheese, and processed meats.
Minimize Alcohol
While a glass of wine may seem harmless, alcohol can trigger headaches in some people. It’s best to consume alcohol in moderation, if at all.
Avoid Medication Overuse
It’s important to restate that over-reliance on painkillers can lead to a condition called medication-overuse headache. Always follow your healthcare provider’s advice regarding medication use.
Keep a Headache Diary
Another critical step in managing migraines is learning to identify what triggers them.
By keeping a headache diary, you can track your symptoms and identify potential triggers, a crucial step in formulating an effective treatment plan.
These lifestyle modifications can serve as your first line of defense against headaches. Everyone is unique, and what works for one person may not work for another. So, don’t be disheartened if you don’t see immediate results.
Key Takeaways
- Common primary headache types include tension headaches, migraines, cluster headaches, and cervicogenic headaches.
- Tension headaches are often due to stress, poor posture, or sleep issues, and are more common in women, particularly as they age.
- Migraines are severe, often one-sided headaches with symptoms like nausea and light sensitivity, triggered by factors like stress and hormonal changes.
- Cluster headaches are intense, recurrent headaches affecting more men than women, linked to genetics, smoking, and alcohol use.
- Cervicogenic headaches originate from neck disorders and mimic migraines or tension headaches.
- Key factors increasing headache risk include dehydration, hunger, medication overuse, sleep problems, and mental health issues.
- Imaging studies like CT and MRI scans are used for detailed internal views for headache diagnosis.
- Treatments for headaches vary from over-the-counter pain relievers to prescription medications, with attention to avoiding medication overuse.
- Lifestyle changes, such as regular exercise, good posture, stress management, and healthy eating, are crucial in managing headaches.
Resources
- https://www.amjmed.com/article/S0002-9343(17)30932-4/fulltext
- https://www.mayoclinic.org/diseases-conditions/cluster-headache/diagnosis-treatment/drc-20352084
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5974268/
- http://www.mayoclinic.org/diseases-conditions/migraine-headache/basics/risk-factors/con-20026358
- http://www.mayoclinic.org/diseases-conditions/tension-headache/basics/risk-factors/con-20014295






