The pelvic floor is a group of muscles and tissues supporting the pelvis’s organs. This critical structure helps with various daily functions. Unfortunately, it is common for seniors to experience pelvic floor dysfunction, which can lead to a host of problems.
It can be affected by many factors, causing problems such as pain, leakage, prolapse, and sexual dysfunction.
In this article, you will learn to tell if you have pelvic floor problems. You’ll understand what causes them and how to treat them with exercise and the help of a physical therapist.
Let’s explore how you can improve your health by caring for your pelvic floor.
What is the Pelvic Floor?
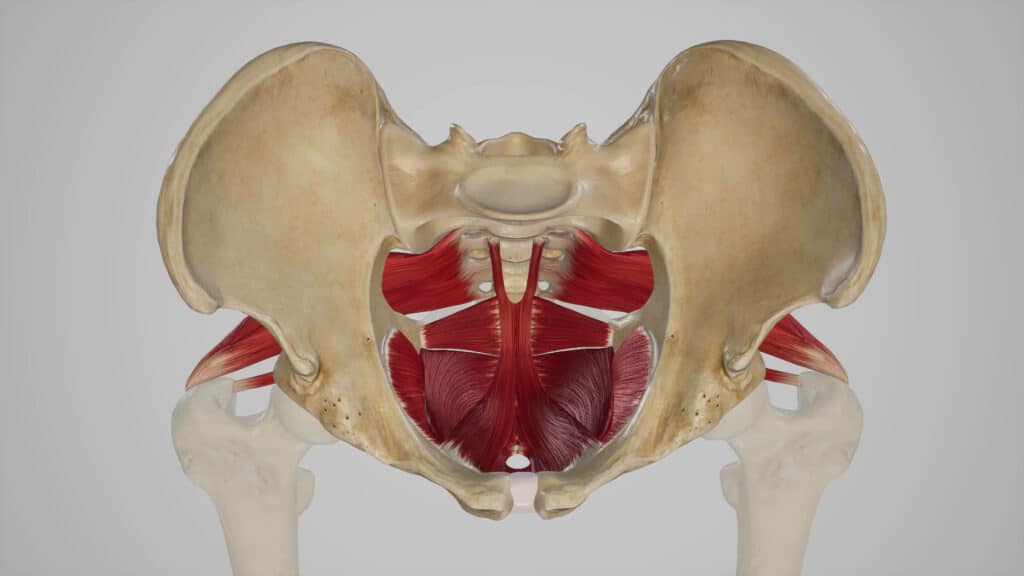
The pelvic floor is a group of muscles, ligaments, and fascia in the pelvis. It has three layers and forms a sling. This structure supports the organs in the pelvis, including the urethra, bladder, rectum, and reproductive organs.
The pelvic floor also helps us with urination, bowel movements, sex, core stability, and balance. The pelvic floor is involved in many of our body’s daily functions.
How the pelvic floor works
The pelvic floor muscles work both voluntarily and involuntarily. They contract to prevent leakage of urine or feces when we cough or exercise. They also relax to allow urination and bowel movements.
The pelvic floor’s performance depends on the coordination of the muscles, the anatomy of the pelvic region, and the strength of the tissues.
What affects our pelvic floor
Many factors can impact our pelvic floor’s health and function.
These include muscle imbalances, aging, menopause, pregnancy, childbirth, back and hip pain, stress, hypermobility diseases, cancer treatments, surgeries in the abdomen, chronic coughing, eating disorders, and obesity.
As a result, pelvic floor muscles can become too tight, weak, or uncoordinated, which can lead to pelvic floor dysfunction.
Pelvic Floor Dysfunction

Pelvic floor dysfunction occurs when the pelvic floor muscles are not working correctly. This can cause various symptoms, including bowel or bladder incontinence, poor urine retention, constipation, difficulty and pain with sex, organ prolapse, and pelvic and joint pain.
Pelvic pain is a common symptom of pelvic floor dysfunction. According to the International Pelvic Pain Society, it affects around 25 million women in the US, but it can also affect men. It can occur in one or more pelvic areas, including the lower back, hip, rectum, or genitals.
Evaluating the Pelvic Floor
Diagnosing and treating pelvic floor dysfunction may require a team of practitioners. Your primary care doctor can start the process but may refer you to a specialist for further evaluation and testing.
- Urologists specialize in urinary tract problems.
- Urogynecologists specialize in female pelvic health and reconstructive surgery.
- Gastroenterologists specialize in digestive system problems
- Gynecologists/obstetricians specialize in female reproductive health and pregnancy.
The Role of a Pelvic Floor Therapist
Your primary care doctor may also suggest that you start treatment with a pelvic floor therapist first. A pelvic floor therapist is a physical or occupational therapist who has undergone advanced training specific to pelvic floor dysfunction. They will listen to your concerns and symptoms and tailor their evaluation accordingly.
Your evaluation will examine your posture, how you move, how well your pelvic floor functions, and your lifestyle. It will also address the surrounding joints like your hips and lower back. Their primary goal of therapy will be to get you back to enjoying life. This means minimizing or resolving the impact of your pelvic floor dysfunction so you can feel better.
Related Posts
- Should I Avoid Getting on the Floor?
- When Back Pain Isn’t Just Back Pain
- Preventing Falling in the Bathroom
- What Is Core Strength, Anyway?
- The Best Sitting Positions for Lower Back Pain
When treating pelvic floor issues, it’s common to discover other underlying related problems. Patients often arrive with one complaint and discover they have more than one problem that involves their pelvic floor.
For example, I treated a 73-year-old woman seeking treatment due to leaking urine and more frequent trips to the bathroom. In her treatment, we discovered that her pelvic floor disorder was also involved in her chronic constipation and pain with sex that had been affecting her for years.
Common Diagnoses of Pelvic Floor Dysfunction

Some of the common diagnoses of pelvic floor dysfunction include:
- Pelvic pain conditions: vaginismus, vulvodynia, or chronic pelvic or rectal pain.
- Pelvic organ prolapse
- Overactive bladder or painful bladder syndrome/interstitial cystitis
- Urine or fecal incontinence, constipation
- Birth trauma or sexual dysfunction (painful sex, erectile dysfunction)
- Endometriosis
Your pelvic floor therapist will quickly determine whether or not your pelvic floor is working too much.
Sometimes, our pelvic floor will work too hard, leading to muscle tightness, dysfunction, and pain. Other times, our pelvic floor is weak and is unable to perform fully, which can also lead to pain and dysfunction.
Exercises for the Pelvic Floor
Pelvic floor muscle exercises emphasize strengthening, stretching, and relaxation of the pelvic floor and other muscles surrounding the pelvis.
A Brief Guide to Kegel Exercises

Kegel exercises, also known as pelvic floor exercises, involve repeatedly contracting and relaxing the muscles that form part of the pelvic floor, sometimes called the “Kegel muscles.” These exercises can be done while standing, seated, or in a bridge position, as seen in the image above.
The aim is to strengthen these muscles, which support the uterus, bladder, small intestine, and rectum.
For all genders, this can help improve bladder and bowel control and can enhance sexual function. To perform Kegel exercises, one must identify the correct muscles, which can be found by trying to stop urination mid-flow.
Once identified, these muscles are contracted for three to five seconds and then relaxed for three to five seconds. Doing these exercises three times daily is generally recommended, performing about 10 to 15 repetitions each time.
During the exercise, it’s essential not to contract other muscles like the stomach, buttocks, or legs. Kegels can be done discreetly and without any special equipment, making them a convenient and accessible way to maintain pelvic floor health.
The Role of Coordination
Strengthening exercises like Kegels are appropriate if weakness is the cause of your symptoms. But if your muscles are too tight, Kegels can make your pain worse. Exercises must emphasize control and coordination for successful rehabilitation of the pelvic floor.
Proper coordination is essential to strengthen the pelvic floor. Each contraction should be followed by complete relaxation of the muscles. It’s also important to isolate the pelvic floor rather than the surrounding larger muscles.
For men, you should feel your muscles draw your genitals up and in. For women, the muscles around your vagina and rectum muscles will pull up and in. Hold the muscle tight for as long as you can comfortably and correctly, and repeat for ten repetitions. Initially, you may only be successful for a couple of seconds. Gradually work on increasing your hold time for up to 10 seconds.
If you are unsure if you are doing them correctly or are experiencing pain, stop and seek treatment with a pelvic floor therapist.
Special Considerations
Examining why your pelvic floor is not working optimally for the best recovery is imperative. Again, this is very specific to your symptoms.
For example, suppose you are experiencing trouble holding your urine and making it to the bathroom quickly. In that case, dietary and lifestyle factors may contribute. Education on behavior changes in conjunction with your strengthening program will be the best way to eliminate your symptoms and prevent them from returning.
Low back and hip pain or weakness can also interfere with how well the pelvic floor works. Treatment of these areas should be included in the plan you develop with your PT.
Pelvic Floor Hope
I have noticed a tendency for people to assume symptoms like loss of bladder control or difficulty with sex are something you have to live with. But these are not hopeless signs that you’re getting older or going through menopause.
The good news is that we have multiple treatment tools to address any and all of these problems. Pelvic floor therapy can be one of the first lines of treatment for various pelvic floor disorders.
With knowledgeable help, pelvic floor issues can be treated successfully. Proper treatment can improve your quality of our life, no matter what stage of life we are at.
Key Takeaways
- The pelvic floor is a crucial set of muscles, ligaments, and fascia that support various biological functions in the pelvis.
- Its dysfunction can manifest in various ways, from pain and leakage to sexual discomfort.
- Lifespan-related factors such as pregnancy, aging, and surgeries can impact pelvic floor health.
- Diagnosis often involves multiple specialists, and treatment can range from exercises to specialized therapy.
- It’s essential to understand the nature of the dysfunction. Determining whether the muscles are too tight or weak to effectively target the treatment is key.
- Pelvic floor therapy offers hope for people struggling with these problems. Therapy emphasizes that many issues are not inevitable parts of aging or other life stages.
FAQs
Why is it crucial to maintain a healthy pelvic floor?
Maintaining a healthy pelvic floor is essential for several reasons beyond the commonly acknowledged prevention of incontinence.
The pelvic floor muscles are instrumental in supporting the pelvic organs, contributing to core strength and stability, and ensuring proper balance. They also play a crucial role in sexual function, where a strong pelvic floor can enhance sensation and orgasmic potential, contributing positively to sexual health and satisfaction.
Are men affected by pelvic floor issues?
Pelvic floor issues are not exclusive to women; men are equally susceptible to pelvic floor dysfunction, although it is less frequently discussed in male health conversations.
In men, pelvic floor dysfunction can lead to chronic prostatitis, which is the inflammation of the prostate gland, or contribute to erectile dysfunction, impacting sexual health and urinary function.
Is age the primary factor in pelvic floor problems?
While aging contributes to pelvic floor weakness due to the natural loss of muscle tone and elasticity over time, it is not the sole cause.
Younger individuals may also experience pelvic floor problems due to factors such as injury, certain high-impact sports, surgical procedures like prostatectomy or hysterectomy, or conditions such as obesity, which place additional stress on these muscles.
Can exercises worsen pelvic floor issues?
Exercises aimed at strengthening the pelvic floor, such as Kegels, can indeed exacerbate issues if performed incorrectly.
Overworking the pelvic floor muscles without proper relaxation can lead to a condition known as hypertonicity, where the muscles become too tight, causing pain, discomfort, and even functional problems. A balanced approach incorporating strengthening and relaxation exercises is critical for maintaining a healthy pelvic floor.
Are there non-surgical treatments available for pelvic organ prolapse?
For those dealing with pelvic organ prolapse, there are several non-surgical treatment options available. While advanced cases may necessitate surgical repair, many people with milder symptoms find relief through targeted pelvic floor physical therapy, which can help strengthen the muscles and support the organs.
Lifestyle modifications can also be beneficial, such as weight management and avoiding activities that increase intra-abdominal pressure. Additionally, medical devices such as pessaries are non-surgical options that support the prolapsed organs and can be a suitable treatment for specific individuals.
References
- Bo K., Berghmans B., Morkved S., Van Kampen M. Evidence-based physical therapy for the pelvic floor: Bridging science and clinical practice 2nd edition Elsevier Churchill Livingstone 2015
- Bump R.C., Norton P.A., Epidemiology and natural history of pelvic floor dysfunction Obstetrics & Gynecology Clinics 1998;25(4):723–746
- Dorey G., Pelvic Floor Exercises for Erectile Dysfunction Whurr Publishers Ltd 2004
- Dumoulin C., Hay-Smith J., Mac Habée-Séguin G. Pelvic Floor Muscle Training Versus No Treatment or Inactive Control Treatments for Urinary Incontinence in Women. Cochrane Database Syst Rev 2014;5:CD005654
- Hagen S., Stark D., Conservative prevention and management of pelvic organ prolapse in women Cochrane Database Syst Rev 2011;12:CD003882
- Hay-Smith E.J.C., Bo K., Berghmans L.C.M., Hendriks H.J.M., de Bie R.A., van Waalwijk van Doorn E.S.C., Pelvic Floor Muscle Training for Urinary Incontinence in Women Cochrane Database Syst Rev 2001;1:CD001407
- Lowenstein L., Gruenwald I., Gartman I., Vardi Y., Can stronger pelvic muscle floor improve sexual function? Int Urogynecol J Pelvic Floor Dysfunct 2010;21(5):553–556
- Messelink B., Benson T., Berghmans B., Bo K., Corcos J., Fowler C., et al. Standardization of terminology of pelvic floor muscle function and dysfunction. report from the Pelvic Floor Clinical Assessment Group of the International Continence Society Neurourol Urodyn 2005;24(4):374–380
Reilly E.T.C., Freeman R.M., Waterfield M.R., Waterfield A.E., Steggles P., Pedlar F. Prevention of postpartum stress incontinence in primigravidae with increased bladder neck mobility. a randomised controlled trial of antenatal pelvic floor exercises BJOG 2002;109(1):68–76
- Thakar R., Sultan A.H., Pelvic organ prolapse: a practical guide Springer International Publishing Switzerland 2016





