Have you ever experienced a sharp, stabbing pain in your heel when you take your first steps in the morning? Or perhaps you’ve felt a persistent ache in the arch of your foot that won’t go away.
If so, you might be among the millions of active adults who have encountered a common yet often misunderstood foot condition called plantar fasciitis.
Plantar fasciitis can affect anyone, and its discomfort can be debilitating. In the following sections, we will demystify plantar fasciitis to offer a clear understanding of what it is and practical strategies for relief and recovery. This short guide will help you navigate the ins and outs of plantar fasciitis so that you can find relief.
What is Plantar Fasciitis?
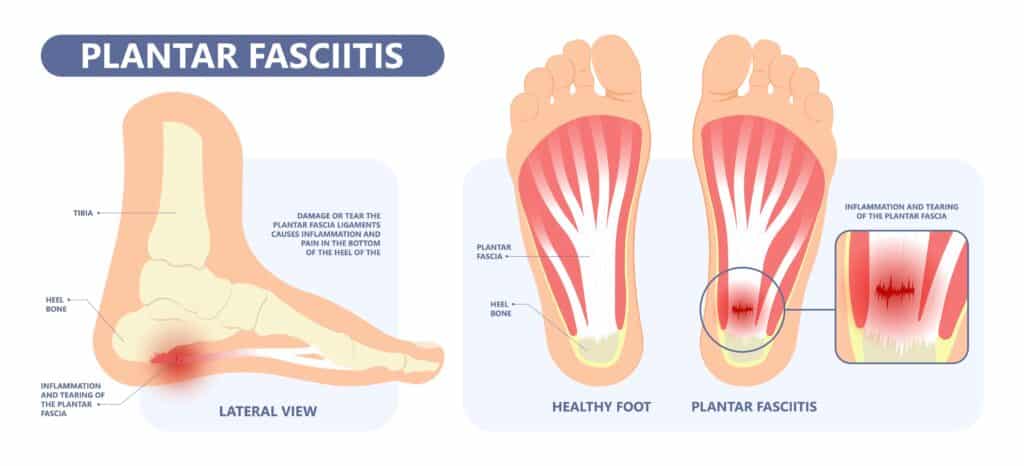
Despite its complex-sounding name, plantar fasciitis is quite simple: it’s an inflammation of the plantar fascia, an essential structure in your foot. But what exactly is the plantar fascia, and why is it so important?
The Plantar Fascia
The plantar fascia is a thick, fibrous, web-like band of tissue that runs along the entire bottom of your foot, connecting your heel bone to each of your toes. Its primary role is to support the arch of your foot, protect the individual muscle tendons, and provide stability by helping you maintain proper balance.
The plantar fascia experiences immense stress and heavy load every day. Every step you take involves this crucial structure. Over time, this constant strain can lead to tiny tears in the plantar fascia, causing inflammation and pain. It’s like a resilient cable, but even the toughest cables can fray under pressure.
Causes and Risk Factors
Understanding what triggers plantar fasciitis is the first step in preventing and managing it effectively. Let’s explore the common causes and who’s most likely to find themselves dealing with this condition.1
Plantar fasciitis often develops due to a combination of factors, including:
- Overuse: Engaging in activities that place excessive stress on the feet, such as running or standing for long hours, can strain the plantar fascia.
- Improper Footwear: Ill-fitting shoes, especially those lacking proper arch support, can contribute to the development of plantar fasciitis.
- Age: Our tissues can become less flexible as we age, making them more prone to injury.
- Weight: Carrying excess body weight increases the stress on the plantar fascia.
While plantar fasciitis doesn’t discriminate, some individuals are more susceptible. You might be at a higher risk if you:
- Are Over 40 years old: Age-related changes to the makeup and elasticity of your soft tissue can make the plantar fascia less flexible.
- Engage in High-Impact Activities: Athletes and individuals with jobs that require prolonged standing are more prone to developing the condition.
- Have Flat Feet or High Arches: An abnormal foot structure can contribute to the problem.
- Wear Ill-Fitting or Worn-Out Shoes: High heels and shoes without proper arch support do not benefit your foot health. Also, shoes that are worn out tend to contribute to incidences of PF.
Identifying the Symptoms

As with any medical condition, early recognition of the signs and symptoms of plantar fasciitis can make a significant difference in treatment and recovery. Let’s look at the key indicators of this ailment and why it’s crucial to identify them promptly.
Early Warning Signs
The early stages of plantar fasciitis can be subtle, often mistaken for general foot discomfort. However, paying attention to the evolution of these initial signs can be pivotal (1, 2).
The most notable symptom of plantar fasciitis is sharp pain at the bottom of your heel. This pain is usually most pronounced with your first steps in the morning or after periods of rest.
Some of my patients report that they also experience pain in the middle of the foot, particularly along the arch. The exact pain location will depend on your anatomy, so pay attention to how your foot feels throughout the day and note patterns of discomfort in specific areas.
Pain may worsen after prolonged standing, walking, or exercising. And you might notice a feeling of stiffness in your foot, especially after periods of inactivity.
Early recognition of these symptoms is vital for several reasons. Plantar fasciitis can significantly impact your daily activities and overall quality of life. It can also worsen slowly, which can cause gradual, imperceptible changes in how you move.
The sooner you identify plantar fasciitis, the quicker you can begin treatment, which often leads to faster relief. Ignoring initial discomfort can allow the condition to worsen, making it more challenging to manage.
Diagnosis of Plantar Fasciitis
While recognizing the symptoms is the first step, a definitive diagnosis often requires the expertise of a medical professional. Your healthcare provider may use several tests to determine your PF.
Typically, screening involves a physical examination of your foot and a discussion of your symptoms. This might include reviewing your medical history, activity level, and recent injuries.
X-rays or other imaging tests may be used to rule out other possible causes of your pain, such as hairline or stress fractures. In some cases, an ultrasound or MRI can provide a more detailed view of the plantar fascia.
Self-diagnosis can be challenging, and many foot conditions share similar symptoms. Seeking professional guidance ensures you receive an accurate diagnosis and a tailored treatment plan.
Treatment Options
Managing plantar fasciitis effectively often involves a combination of approaches tailored to your condition. In this section, we’ll explore various treatment options, ranging from conservative methods to more advanced medical interventions.
Common At-Home Options
Rest, Ice, Compression and Elevation (RICE)
When managing plantar fasciitis, sometimes less is more. Resting the affected foot, applying ice to reduce inflammation, and elevating your foot can provide much-needed relief. The ‘C’ refers to compression, which may be helpful in some cases.
More recently, the acronym POLICE has been embraced by physical therapists, referring to Protection, Optimal Loading, Ice, Compression, and Elevation. Note that protection and optimal loading indicate that rest may not always be the best treatment, as moving the tissues is often beneficial to healing.
Consult your physical therapist to determine the best approach to treat your condition in its initial stages.
Footwear and Orthotics
The correct footwear can make a world of difference. Supportive shoes with proper arch support and cushioning can alleviate strain on the plantar fascia. Orthotic insoles or custom-made orthotics can also be beneficial.
I encourage my patients to wear supportive shoes (not slippers) in the house and avoid being barefoot if possible during the beginning, painful stages of the condition. Talk to your doctor if you want to explore orthopedic footwear for plantar fasciitis or other related conditions.
Physical Therapy
Physical therapy plays a crucial role in the rehabilitation of plantar fasciitis. A PT can assess your condition and tailor a treatment plan to your needs.
As medical professionals, we offer our patients specific exercises and stretches to strengthen the muscles supporting the foot and improve flexibility. Your PT can give you feedback on your performance of these exercises and design a home exercise program that helps you meet your rehabilitation needs safely and effectively.
In my practice with patients with plantar fascitis, I also perform hands-on techniques to reduce pain and inflammation, including soft tissue massage and mobilizations to the structures in and surrounding the foot.
Here are some exercises and stretches I often recommend to my patients:
Calf & Achilles Tendon Stretch
This stretch across the back of the ankle joint targets the calf muscles and tendon, which can contribute to plantar fasciitis when tight. Stand facing a wall with both hands on the wall. Step one foot back, keep your leg straight, and bend the front knee. This will allow you to feel a stretch in the back of your lower leg and ankle.
Big Toe Plantar Fascia Stretch
Gently stretching the plantar fascia itself can provide relief. You can do this by keeping your foot flat and pulling your big toe up and away from the floor. You can also perform this stretch in a figure 4 position if that is more comfortable for you, as seen in the video above.
Tennis Ball Mobilization
Sit in a chair with your foot resting on a small ball, such as a tennis ball. Applying some mild downward pressure from your foot onto the ball, gently roll the ball around, moving it from the ball of your foot to your heel. Perform with only enough pressure that gives you a stretching sensation, not pain.
Alternatively, you can freeze a plastic water bottle and roll it between the arch of your foot and the floor to provide the benefits of icing.
To complement exercises and stretches, you can also consider using night splints. This device stretches the foot and toes while sleeping to aid in treating PF.
Surgery or Medical Intervention
Over-the-counter pain relievers or prescription medications may sometimes be recommended to manage pain and inflammation. Corticosteroid injections can temporarily relieve severe pain and inflammation but are typically used sparingly due to potential side effects.
Surgery is generally considered a last resort when all other treatments have failed to provide relief, and the pain remains severe and debilitating. Surgical procedures for plantar fasciitis typically involve releasing or removing the damaged tissue. (3)
Surgery, like any medical procedure, carries significant risks. It’s essential to have a thorough discussion with your healthcare provider to weigh the potential benefits of surgery against the risks and ensure it’s the right course of action for your specific case.
Exercises for Plantar Fasciitis
Recovery from plantar fasciitis isn’t limited to medical treatments alone; at-home exercises can play a significant role in your healing journey. There are a range of exercises and lifestyle changes that you can incorporate into your daily routine to find relief.
Strengthening Exercises
You can incorporate any stretches and strengthening exercises mentioned above that are common for physical therapists to prescribe.
Strengthening the muscles in your feet can support the plantar fascia, and stretching can allow for decreased tightness and stiffness. Here are some additional exercises I often offer to my patients that are simple enough to perform at home:
Toe Yoga
Toe yoga is a simple and effective practice involving various exercises and stretches with your toes to improve their flexibility, intrinsic strength, and overall health. This includes exercises such as toe spreading, toe gripping, and toe extensions.
Arch Lifts
Keep your toes and heel on the ground and raise the arch of one foot by curling your toes upward. Imagine you’re trying to create a “dome” shape with your foot’s arch.
Towel Scrunches
Place a small towel on the floor and use your toes to scrunch it toward you. Repeat until you feel fatigue in the arches of your feet, rest and repeat.
Other Simple Exercises You Can Do Today
- Marble Pickup: Place marbles on the floor and use your toes to pick them up, and place them in a container.
- Toe Tapping: Sit in a chair with your feet flat on the ground and tap your toes rapidly for 30 seconds.
In addition to strengthening exercises, improving balance and flexibility can help reduce the risk of injury and improve overall foot health. Consider practices like Tai Chi or yoga, which emphasize balance and flexibility. If tolerable, single-leg balance exercises can help work on intrinsic foot strength, which aids in decreasing the overall stress and load on the plantar fascia.
Prevention and Long-Term Care

Recovering from plantar fasciitis is significant, but the journey doesn’t end there. Adopting preventive measures and establishing a long-term foot care routine is essential to ensure lasting relief and minimize the chances of recurrence.
Lifestyle Changes
While there are some more comprehensive treatment methods available
Proper footwear is essential in avoiding PF. If you can wear shoes with more supportive soles, such as shoes designed for running or walking, they can significantly help decrease your foot pain. Though there is a time and a place for being barefoot to work on your general foot strength, take breaks to wear shoes with good support to keep pain under control. Additionally, if you work on your feet all day, take a few seated rest breaks or take some time to do some of the described stretches above at intervals throughout the day. (3)
Carrying excess body weight places additional stress on your feet, exacerbating the symptoms of plantar fasciitis. Maintaining a healthy weight through a balanced diet and regular exercise can significantly reduce the strain on your feet and aid recovery.
Incorporating these at-home exercises and lifestyle changes into your daily routine can complement your treatment plan and contribute to a speedier recovery from plantar fasciitis.
Preventing Recurrence
Lifestyle Modifications for Preventing Future Episodes: Once you’ve successfully managed plantar fasciitis, here’s how to reduce the risk of it returning:
- Maintain a Healthy Weight: If you’ve seen improvement in your foot health with some body weight loss, continue to focus on maintaining that healthy-for-you weight.
- Gradual Activity Increase: When returning to physical activities, do so gradually. Don’t rush back into high-impact exercises. Oftentimes, a sudden increase is what caused an injury in the first place.
- Proper Footwear: Stick to supportive shoes with good arch support and cushioning. Avoid flat, high-heeled, or unsupportive footwear.
- Regular Stretching: Continue with daily stretches to keep your calf muscles, Achilles tendon, and plantar fascia flexible.
- Strength Training: Maintain foot muscle strength through the calf, leg, hip, and intrinsic foot muscle exercises.
Take care of your feet before discomfort returns: incorporate some of the abovementioned practices into your daily routine. Light morning stretches before taking your first steps can help to decrease that classic plantar fasciitis pain.
You can perform a stretch like the calf stretch or the plantar fascia stretch for the foot arch while still in bed to gently wake up the soft tissue in your affected foot. That way, you allow your foot structures to warm up before your entire body weight bears down on your arches.
Regular self-massage can also help alleviate tension and discomfort. You can perform this first thing in the morning before leaving bed. Still, it is also suitable after a shower or right before sleep to relieve tension after a long day.
When to Seek Professional Help
While self-care is crucial, knowing when to seek professional assistance is equally important. Consult a healthcare provider if you experience severe or prolonged pain or if your pain worsens or doesn’t improve with conservative treatments. Additionally, a medical expert should evaluate any new or unusual symptoms in your feet. Finally, I always remind my patients that if they notice redness, swelling, or signs of infection in the affected foot, they should seek immediate medical attention.
Just as you schedule regular check-ups with your primary care physician, consider routine foot care appointments, especially if you’ve had foot issues. A podiatrist can provide expert guidance and identify potential problems before they become severe.
By adhering to these preventive measures and knowing when to seek professional help, you can take proactive steps to keep plantar fasciitis at bay and enjoy a life free from foot discomfort.
Key Takeaways
- Plantar fasciitis is characterized by heel pain and can be managed with early detection and treatment.
- Common causes include overuse, improper footwear, age-related changes, and excess weight.
- Early warning signs include morning heel and arch pain, prompting the need for a professional diagnosis.
- Treatment options include rest, ice, physical therapy, and, in severe cases, medical interventions or surgery.
- At-home exercises like stretching and strengthening can complement treatment and prevent recurrence.
- Long-term care involves lifestyle modifications, regular foot care, and seeking professional help.
References:
- Tahririan, M. A., Motififard, M., Tahmasebi, M. N., & Siavashi, B. (2012). Plantar fasciitis. Journal of Research in Medical Sciences: the official journal of Isfahan University of Medical Sciences, 17(8), 799.
- Digiovanni, B. F., Nawoczenski, D. A., Malay, D. P., Graci, P. A., Williams, T. T., Wilding, G. E., & Baumhauer, J. F. (2006). Plantar fascia-specific stretching exercise improves outcomes in patients with chronic plantar fasciitis: a prospective clinical trial with two-year follow-up. JBJS, 88(8), 1775-1781.
- Lim, A. T., How, C. H., & Tan, B. (2016). Management of plantar fasciitis in the outpatient setting. Singapore Medical Journal, 57(4), 168.





