Degenerative scoliosis affects many adults, resulting from age-related changes such as disc degeneration, osteoporosis, and arthritis. This condition manifests with symptoms that include lower back pain, changes in posture, and difficulties in walking.
The risk of developing degenerative scoliosis increases with age, lifestyle choices, and previous spinal injuries. Diagnosing this condition requires thorough physical exams and detailed imaging techniques like X-rays and MRIs.
Treatment can range from physical therapy—which incorporates exercises such as the Cat-Cow Stretch and Pelvic Tilts—to surgical interventions for more severe cases. Moreover, educating patients on proper body mechanics is crucial for managing daily activities and enhancing long-term well-being.
Let’s explore each of these aspects to better understand how they contribute to effective management and recovery.
A Primer on Degenerative Scoliosis
As we age, the discs that cushion the vertebrae in our spine can wear out. This wear can decrease disc height and alter the spine’s alignment, eventually causing it to curve or twist—a condition known as scoliosis.
Degenerative scoliosis is a condition that affects adults. It typically develops as a result of age-related changes in the spine. Unlike the scoliosis commonly seen in adolescents, which usually appears during teenage years, degenerative scoliosis occurs later in life.
This form of scoliosis is linked to the natural aging process of the spine, including conditions like disc degeneration, osteoporosis, and spinal arthritis.
Degenerative scoliosis usually progresses slowly and can cause back pain, stiffness, and difficulties with balance and mobility.
Several factors may increase the risk of developing degenerative scoliosis, including age, genetic predisposition, past spinal injuries, and underlying conditions like osteoporosis and spinal arthritis.
Managing degenerative scoliosis focuses on relieving these symptoms, improving mobility, and preventing the curvature from worsening. Treatment options range from conservative approaches like physical therapy, pain management, and bracing to surgical interventions in more severe cases.
Who’s at Risk?
Identifying the risk factors for degenerative scoliosis involves considering several key aspects of an individual’s background and health.
Age plays a critical role in the likelihood of developing this condition. Our spines naturally degenerate as we age, and studies suggest that around 60% of adults over sixty exhibit signs of degenerative disc disease.
Just as aging skin loses moisture and elasticity, leading to wrinkles, the joints in our spine undergo similar changes. Spinal discs dry out, lose height, and become less elastic. This results in diminished shock absorption and increased susceptibility to injuries. Such disc degeneration is a significant factor in developing degenerative disc disease.
Furthermore, the more time we spend living and moving, the more repetitive stress our spines endure from daily activities such as lifting, bending, and twisting. This ongoing strain can cause wear and tear on spinal discs, weakening them and exacerbating degenerative changes.
Lifestyle choices also significantly impact the risk of developing degenerative scoliosis. Factors like smoking, obesity, and a lack of physical activity can hasten disc degeneration.
Smoking, for example, is particularly harmful as it restricts blood flow to the spinal discs, impairing their ability to receive nutrients and repair themselves.
Additionally, previous spinal injuries—such as herniated discs, fractures, or consistent minor traumas—can accelerate the degenerative processes in the spine. These injuries may weaken the structures supporting the spine, including the vertebral and facet joints, compromising their functionality over time.
Recognizing the Symptoms and Complications

Degenerative scoliosis may not always present apparent symptoms initially, and some individuals might not experience any discomfort. However, the severity of symptoms can vary widely, from mild to severe.
The common symptoms of degenerative scoliosis include lower back pain, noticeable changes in posture, and difficulty walking.
Lower back pain typically manifests as a dull, persistent ache that can fluctuate in intensity. This discomfort might be intermittent for some, while others may suffer from continuous chronic pain.
Actions like bending, lifting, or remaining in one position for too long, such as sitting or standing, can intensify this pain.
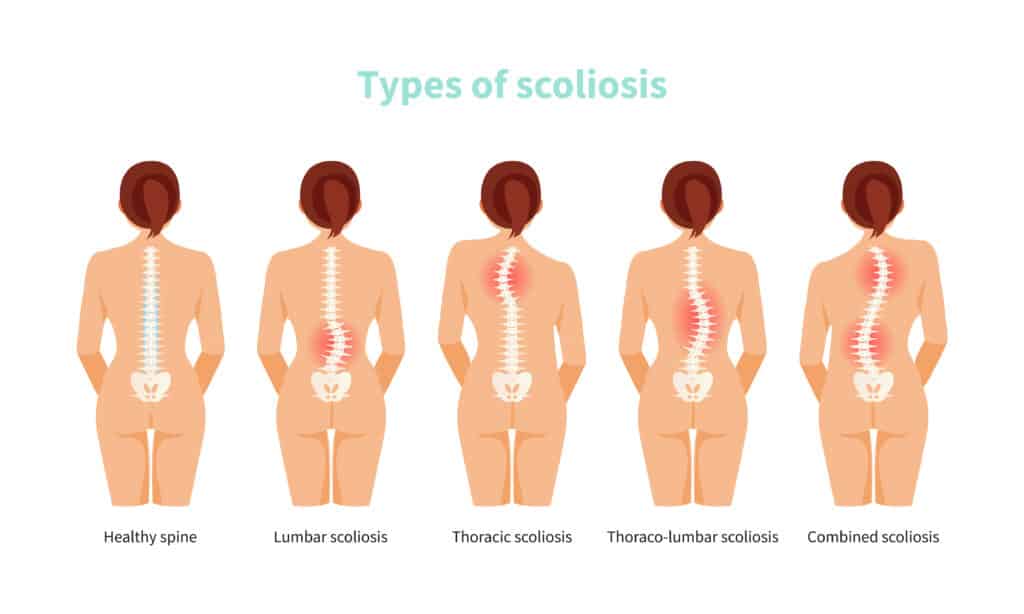
As the condition progresses, changes in spinal alignment, such as an increased curvature of the spine or a forward-leaning posture, become more evident.
These alterations can significantly impact an individual’s posture, potentially leading to visible kyphosis (forward curvature) or scoliosis (sideways curvature). In some cases, both conditions may coexist.
Mobility issues are also common, with individuals experiencing stiffness and muscle imbalances affecting their walking ability. This can compromise comfort and mobility, making it challenging to maintain a regular gait.
As the spine degenerates, it may also compress or irritate nerves, leading to numbness, tingling, or weakness radiating from the lower back into the legs.
In severe scenarios, the cumulative effects of these symptoms can significantly reduce the quality of life, restricting mobility and independence. Chronic pain, mobility limitations, and changes in posture can lead to physical and emotional distress.
Managing these symptoms is crucial for improving spinal function and overall well-being and often requires a comprehensive approach to treatment.
Diagnosing Degenerative Scoliosis
Early diagnosis of degenerative scoliosis is crucial for effectively managing the condition, particularly in older adults. The diagnosis involves several key steps, beginning with a thorough physical examination.
During the initial evaluation, your doctor will examine your back for any signs of abnormal curvature or asymmetry. They may also conduct flexibility tests, asking you to bend in various directions to assess the flexibility of your spine.
However, the examination is just the starting point. The diagnostic process typically includes a variety of imaging tests to gain a clearer picture of your spine’s condition.
X-rays are fundamental in this process, as they provide clear images of the spinal column, highlighting the curvature’s extent and pinpointing areas of spinal degeneration that could contribute to symptoms.
MRIs and CT Scans
MRI scans add another layer of detail, enabling doctors to see beyond the bones to the soft tissues. These scans are beneficial for identifying complications like nerve impingement, pinched nerves, or spinal cord compression, which are common in degenerative scoliosis.
Other imaging techniques, such as CT scans, may also offer a three-dimensional view of the spine, adding further clarity to the diagnosis. Bone scans might be conducted to exclude other bone-related conditions that could mimic or influence the symptoms of degenerative scoliosis.
Understanding the severity and progression of the disease is vital for crafting an effective treatment plan. By assessing the curvature degree and its progression, healthcare providers can customize treatments ranging from physical therapy and pain management to surgical intervention in more severe cases.
Since degenerative scoliosis typically progresses slowly, ongoing assessments are essential to monitor changes and adapt the treatment strategy as needed.
Diagnosing degenerative scoliosis goes beyond merely identifying the condition—it’s about understanding it in depth to minimize discomfort and maximize quality of life.
As a patient, being proactive, asking questions, and expressing concerns are crucial parts of your healthcare journey. They help ensure that treatment plans are as effective and responsive as possible.
Treatment Options for Degenerative Scoliosis
The treatment of degenerative scoliosis is designed to alleviate symptoms, enhance spinal function, and improve the overall quality of life. Treatment choices depend on several factors, such as the severity of symptoms, the degree of spinal curvature, and the individual’s overall health and lifestyle.
Conservative Treatments
Initially, conservative methods are generally recommended. These include physical therapy to strengthen the muscles that support the spine, enhance flexibility, and promote better posture.
Physical therapists create personalized exercise programs tailored to patients’ needs and limitations. These exercises focus on improving core strength, spinal mobility, and postural alignment, which are crucial for managing pain and improving function.
Pain management strategies are another cornerstone of conservative treatment. These may involve over-the-counter or prescription medications to help ease the discomfort of degenerative scoliosis.
Nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, and analgesics are commonly used to reduce inflammation, relax muscle spasms, and lower pain levels, making daily activities more manageable.
In some instances, bracing may be suggested to provide external support to the spine and help stabilize its curvature.
While braces do not correct the curvature, they can slow its progression and alleviate symptoms, especially during physical activity. This option is often used for individuals with moderate scoliosis who are still experiencing changes in their spine or worsening symptoms.
Surgical Intervention
For those with severe or progressive degenerative scoliosis that significantly impairs quality of life and functionality, surgical options may be considered. Spinal fusion surgery is the most common surgical treatment for this condition.
During this procedure, the affected vertebrae are fused together using bone grafts and implants to stabilize the spine and reduce pain. The specific surgical approach may vary based on the curvature’s characteristics and the patient’s overall health.
The treatment plan for degenerative scoliosis typically involves a multidisciplinary approach, including orthopedic surgeons, physical therapists, pain management specialists, and other healthcare professionals.
The aim is to customize the treatment to meet each patient’s unique needs, considering their symptoms, functional limitations, and preferences to optimize outcomes.
Regular follow-up appointments are essential to evaluate the treatment’s effectiveness, monitor the disease’s progression, and adjust the treatment plan as necessary, ensuring the best possible management of the patient’s condition.
The Vital Role of Physical Therapy in Managing Degenerative Scoliosis

Physical therapy is integral in managing the pain and discomfort associated with degenerative scoliosis. As a medical expert and physical therapist, I have observed its profound impact on patients’ quality of life.
The Goals of Physical Therapy
The focus is on strengthening the muscles supporting the spine, enhancing flexibility, and improving posture. These goals are crucial as they help manage pain and potentially slow the progression of scoliosis.
Studies have shown that targeted physical therapy programs can significantly enhance functionality and reduce pain in older adults with this condition.
In practice, I work closely with patients to understand their pain points, limitations, and objectives. This dialogue is vital for developing a practical and effective therapy plan.
Through physical therapy, patients can achieve improved spinal stability and reduced discomfort, enhancing their ability to perform daily activities and improving their overall quality of life.
Therapeutic exercises often focus on core strengthening, spinal mobility, and alignment correction, all geared towards alleviating pressure on the spine and enhancing the patient’s physical capacity.
Physical therapy provides a strategic, tailored approach that addresses the symptoms and contributes to a longer-term improvement in health and functionality. This patient-centered treatment is vital for managing the condition effectively and ensuring each patient can lead a more comfortable and active life.
Exercise and Education in Managing Degenerative Scoliosis
Therapeutic exercises form a crucial component of the treatment plan for degenerative scoliosis. These exercises are tailored to strengthen the muscles supporting the spine, enhance flexibility, and promote better posture.
They range from simple stretches to more sophisticated exercises using specific equipment to alleviate pain and prevent further degeneration.
Recommended Exercises for Degenerative Scoliosis
Cat-Cow Stretch
- Start on your hands and knees with your wrists aligned under your shoulders and your knees under your hips.
- Inhale as you arch your back, lifting your chest and tailbone towards the ceiling, creating a concave curve in your spine (cow position).
- Exhale as you round your spine, tucking your chin towards your chest and pressing your hands and knees into the floor, creating a convex curve in your spine (cat position).
- Repeat this sequence, flowing smoothly between cow and cat positions for 8-10 repetitions.
Pelvic Tilts
- Lie on your back with your knees bent and feet flat on the floor, hip-width apart.
- Inhale to prepare, then exhale as you gently tilt your pelvis backward, flattening your lower back against the floor.
- Hold this position for a few seconds, feeling a gentle stretch in your lower back.
- Inhale as you return to the starting position, allowing a natural arch to return to your lower back.
- Repeat this movement for 8-10 repetitions, focusing on controlled and fluid movements.
Bird-Dog Exercise
- Begin on your hands and knees, ensuring your hands are under your shoulders and your knees under your hips.
- Extend your right arm forward and stretch your left leg back, keeping both parallel to the floor.
- Hold this position for a few seconds, then return to the starting position.
- Switch sides, extending your left arm and right leg.
- Perform this exercise for 8-10 repetitions on each side, focusing on maintaining balance and stability.
Bridges
- Lie on your back with your knees bent and feet flat on the floor, about hip-width apart.
- Press your feet into the floor and lift your hips towards the ceiling, squeezing your buttocks as you lift.
- Hold the lifted position for a few seconds, then slowly lower your hips to the floor.
- Repeat this movement for 8-10 repetitions, focusing on using your glutes and core muscles to perform the lift.
Additional Treatment Modalities
Physical therapy often integrates manual therapy techniques, involving hands-on mobilization and spinal manipulation to alleviate pain, improve mobility, and restore function. Many patients find significant relief from these combined approaches, which include exercise, stretching, and manual therapy.
Modalities such as heat, ice, and electrical stimulation also support managing pain and inflammation associated with degenerative scoliosis.
The Importance of Patient Education
Beyond physical interventions, education is a powerful tool in managing degenerative scoliosis. Understanding proper body mechanics and ergonomics enables patients to make informed decisions about their daily activities, reducing spinal strain and managing pain more effectively.
Patients need to apply the principles learned during therapy to their everyday activities. This includes maintaining proper posture, engaging the right muscles during activities, and incorporating recommended movements into daily life for long-term management of their condition.
A comprehensive approach combining exercise, manual therapy, other modalities, and education ensures the most effective management of degenerative scoliosis. This approach aims to enhance patients’ quality of life by reducing pain and improving mobility.
The Power of Personal Stories: Living with Degenerative Scoliosis
Throughout my years in practice, I have witnessed firsthand the transformative impact physical therapy can have on individuals with degenerative scoliosis. One case stands out among the many stories of resilience and recovery, illustrating how profound and beneficial targeted physical therapy can be.
Mark’s Journey with Degenerative Scoliosis
Mark, a 67-year-old retiree, came to my practice burdened by severe lower back pain, a symptom of his recently diagnosed degenerative scoliosis. His mobility was limited, and he had become increasingly dependent on pain medication to manage his daily activities.
Recognizing the challenges he faced, we embarked on a comprehensive physical therapy program aimed at alleviating his pain and enhancing his mobility.
Strengthening focused on his core and lumbar muscles, as well as improving the flexibility of his spine and hips, and enhancing his overall balance.
Such targeted lumbar stabilization exercises have been shown to significantly reduce pain and improve function in older adults with degenerative scoliosis.
Initially, Mark struggled with core engagement, likely due to long-term compensation by surrounding muscles. We began with basic core-strengthening exercises, using tactile and verbal cues to integrate core engagement into everyday activities such as standing from a seated position, getting in and out of his car, and even performing simple household tasks like putting away dishes. This not only helped to reduce his pain but also significantly improved his posture.
After six months of dedicated effort and consistent therapy, Mark experienced a remarkable turnaround. His pain levels substantially decreased, allowing him to dramatically reduce his use of pain medication.
More importantly, he reported significantly improving his quality of life, feeling more independent and capable in his daily routines.
The Impact of Physical Therapy
Mark’s story is a powerful testament to the efficacy of physical therapy in managing degenerative scoliosis. It highlights the potential for individuals to regain a significant portion of their mobility and reduce their pain through dedicated physical intervention.
Personal stories like Mark’s serve as inspiring examples of the positive outcomes that can be achieved. They reinforce the importance of seeking and committing to appropriate therapeutic interventions.
They remind us that with the proper support and treatment, living with degenerative scoliosis can be a journey of recovery and hope.
Key Takeaways
- Degenerative scoliosis typically arises in adults due to age-related spinal changes like disc degeneration, osteoporosis, and arthritis.
- Common symptoms include lower back pain, altered posture, and walking difficulties, which may increase in severity over time.
- Risk factors for developing degenerative scoliosis include aging and genetic predisposition. Lifestyle choices such as smoking, inactivity, and previous spinal injuries also factor.
- Diagnosis involves a physical examination, flexibility tests, and imaging tests like X-rays and MRI scans to assess spine curvature and identify nerve or spinal cord issues.
- Treatment options range from conservative measures like physical therapy and pain management to surgical interventions for severe cases tailored to individual needs based on symptom severity and spine curvature.
- Physical therapy improves spinal stability, flexibility, and overall mobility. It often involves personalized exercises like the Cat-Cow Stretch, Pelvic Tilts, Bird-Dog, and Bridges.
- Patient education on proper body mechanics and ergonomics is vital for daily activity management and long-term symptom control.
- Personal success stories, like Mark’s, highlight the effectiveness of targeted physical therapy in significantly improving the quality of life for those with degenerative scoliosis.
References
- Silva, F. E., & Lenke, L. G. (2010). Adult degenerative scoliosis: evaluation and management. Neurosurgical focus, 28(3), E1.
- Schoutens, C., Cushman, D. M., McCormick, Z. L., Conger, A., Van Royen, B. J., & Spiker, W. R. (2020). Outcomes of nonsurgical treatments for symptomatic adult degenerative scoliosis: A systematic review. Pain Medicine, 21(6), 1263-1275.
- Everett, C. R., & Patel, R. K. (2007). A systematic literature review of nonsurgical treatment in adult scoliosis. Spine, 32(19), S130-S134.




