Understanding Guillain-Barré Syndrome (GBS) provides valuable insights into this rare and serious condition where the body’s immune system mistakenly attacks its own nerves.
In this article, we’ll explore the causes and symptoms of GBS, which often follow infections or other triggers like surgery or, in rare cases, vaccinations. We’ll discuss how neurologists diagnose GBS through specialized tests and how treatments like plasmapheresis and IVIG therapy can help manage symptoms and promote recovery.
Additionally, we’ll highlight the crucial role of physical therapy in restoring strength and mobility, as well as the importance of long-term care and emotional support.
Whether you’re a patient, caregiver, or healthcare professional, this guide offers essential information to better understand and manage GBS.
What is Guillain-Barré Syndrome?
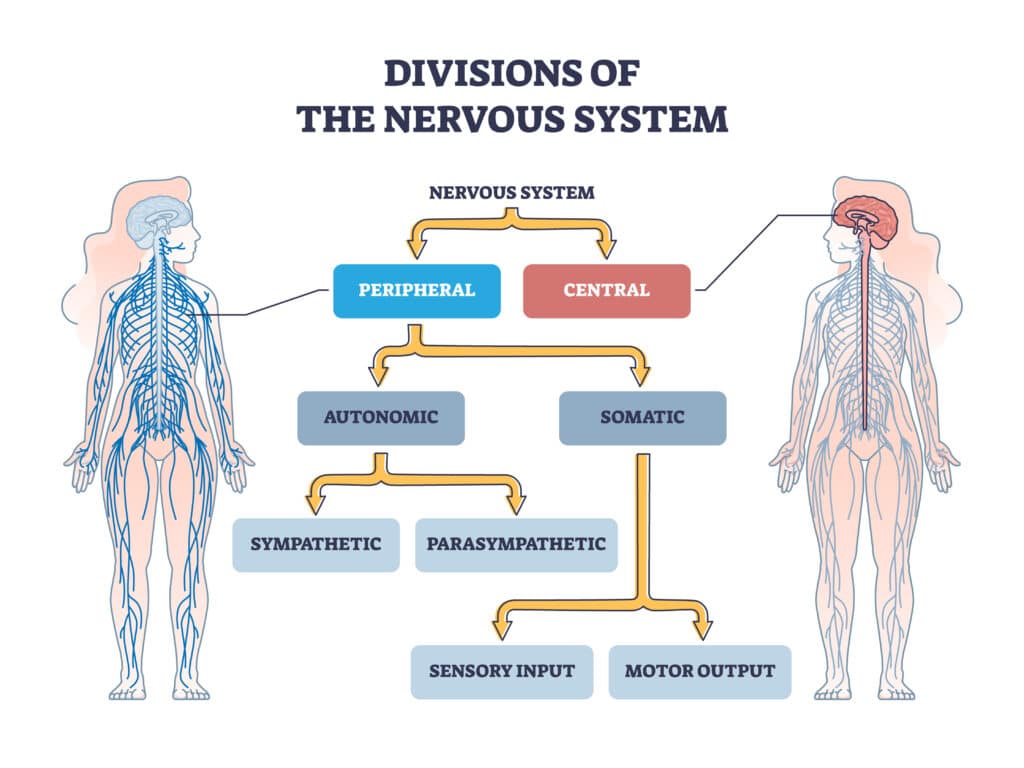
Guillain-Barré Syndrome is a rare but serious condition in which the body’s immune system mistakenly attacks its own peripheral nerves. These nerves are responsible for sending signals from the brain and spinal cord to the rest of the body, and when they are damaged, they can lead to severe problems.
The main signs of GBS include sudden muscle weakness and tingling feelings, usually starting in the legs and feet. This weakness can quickly move to the upper body and arms.
In some cases, the symptoms can get worse in just a few hours or days, causing considerable discomfort and problems. People often describe a pins-and-needles feeling, which can quickly turn into more serious weakness or even paralysis.
In the most severe cases, GBS can affect the muscles used for breathing, leading to breathing failure. This is a medical emergency, and a machine may be utilized to assist with breathing.
Causes and Triggers
The exact cause of Guillain-Barré Syndrome is still not fully understood. However, it is thought to be triggered by an abnormal immune response to certain factors. Often, GBS occurs after an infection, such as a respiratory or gastrointestinal illness.
For example, the bacteria that causes gastroenteritis, an inflammation of the digestive system, is one of the most commonly identified infections linked with GBS.1
Additionally, viral infections like COVID-19, the flu, Zika virus, or Epstein-Barr virus can also come before the onset of GBS.
Other possible triggers include recent surgery, physical trauma, or, in rare cases, vaccinations. While vaccinations can be a potential trigger, the benefits of getting vaccinated to prevent diseases are much greater than the risks of developing GBS.
How is GBS Diagnosed?

Guillain-Barré Syndrome is diagnosed through a comprehensive evaluation conducted by a neurologist. The diagnosis process involves a thorough clinical examination, a review of the patient’s medical history, and a series of specialized tests.
These tests, including lumbar puncture, nerve conduction studies (NCS), and electromyography (EMG), are crucial for confirming the presence of GBS and distinguishing it from other conditions with similar symptoms, like multiple sclerosis or peripheral neuropathy.
These diagnostic tools help accurately identify GBS and assess the extent of the disorder by revealing specific patterns of nerve damage.
Who Diagnoses GBS?
Guillain-Barré Syndrome is usually diagnosed by a neurologist, a doctor specializing in diagnosing and treating nervous system disorders. The diagnosis process includes a clinical examination, reviewing the patient’s medical history, and performing various tests.
These tests might include a lumbar puncture (also known as a spinal tap) to analyze cerebrospinal fluid, nerve conduction studies, and electromyography (EMG) to check nerve and muscle function.
These tests help confirm the diagnosis by revealing specific patterns of nerve damage that are typical of GBS. Let’s have a closer look at the examination and testing process.
Initial Clinical Examination
A thorough physical exam is essential for identifying the symptoms of Guillain-Barré Syndrome. During this exam, a doctor looks for key signs of the disorder, such as muscle weakness, changes in reflexes, and sensory disturbances.
The process starts with a detailed patient history, where the doctor gathers information about recent infections, surgeries, or vaccinations that could be potential triggers.
Next, the doctor conducts a neurological examination, assessing muscle strength and reflexes. Patients with GBS typically show reduced or absent reflexes and muscle weakness that usually starts in the legs and can spread to the arms.
Sensory tests are performed to detect any issues like numbness, tingling, or pain. Tests for coordination and balance may also be done to evaluate the extent of nerve damage.
Additionally, the doctor will check cranial nerve function to see if the facial muscles, eyes, or throat are involved, which can indicate more severe forms of GBS.
These detailed assessments are crucial for identifying weakness and sensory loss patterns that suggest GBS and distinguishing it from other neurological conditions.
Common Diagnostic Tests

Diagnostic tests are essential for confirming Guillain-Barré Syndrome and differentiating it from other conditions with similar symptoms. These tests provide detailed information about the functioning of the nervous system, helping doctors identify key features of GBS and determine the extent of nerve damage.
The main diagnostic tests for GBS include lumbar puncture, nerve conduction studies (NCS), and electromyography (EMG).1
Lumbar Puncture
The lumbar puncture is a key tool for diagnosing GBS and ruling out other conditions with similar symptoms.
A lumbar puncture, or spinal tap, involves inserting a needle into the lower back to collect a sample of cerebrospinal fluid (CSF), which surrounds the brain and spinal cord.
In GBS patients, this test often reveals an elevated protein level in the CSF without an increase in white blood cells. This finding suggests inflammation and damage to the peripheral nerves, as the high protein content indicates the breakdown of the myelin sheath that insulates nerve fibers.
Nerve Conduction Studies (NCS)
Nerve Conduction Studies help doctors understand the extent of nerve damage and the severity of GBS.
This test measures how quickly and strongly electrical signals travel through the peripheral nerves. In GBS, the myelin sheath, which normally helps these signals travel quickly, is damaged.
This damage slows down the signal conduction and reduces the strength of the signals. During the test, small electrodes are placed on the skin over different nerves, and electrical impulses are sent through them.
Electromyography (EMG)
EMG complements NCS by assessing the electrical activity of muscles both at rest and during contraction. To execute this test, a fine needle electrode is inserted into the muscle to record electrical signals.
In GBS patients, EMG may show abnormal spontaneous activity, indicating that the muscles have lost their nerve supply. These results help confirm nerve damage and provide insights into how the muscles respond to nerve signals.
Together, NCS and EMG help pinpoint the type and location of nerve damage, distinguish GBS from other neuromuscular disorders like multiple sclerosis or peripheral neuropathy, and guide treatment decisions.
An EMG can provide a comprehensive evaluation of the peripheral nervous system, ensuring an accurate diagnosis and effective management of GBS.1,2
What to Expect From GBS Treatment
There is no cure for Guillain-Barré Syndrome, but treatments can help manage the symptoms and speed up recovery.
The two main treatments are plasma exchange (plasmapheresis) and intravenous immunoglobulin (IVIG) therapy. Both focus on controlling the immune system to reduce its attack on the nerves.
Plasmapheresis
Plasmapheresis, also known as plasma exchange, involves removing and replacing harmful antibodies from the patient’s blood plasma. This process helps lower the levels of antibodies attacking the nervous system.
Intravenous Immunoglobulin (IVIG)
IVIG therapy involves giving the patient immunoglobulins (antibodies) from healthy donors through an IV. These donated antibodies can block the harmful antibodies in the patient’s body and suppress the immune response, reducing inflammation and nerve damage.
Both plasmapheresis and IVIG have been shown to be effective in improving recovery and shortening the duration of the illness, especially when started early in the course of the disease.
Physical Therapy for GBS

Physical therapy plays a crucial role in rehabilitating patients with Guillain-Barré Syndrome, helping them regain strength, mobility, and independence.
With regular physical therapy, patients can rebuild their muscle strength, improve their balance, and gradually return to normal activities.
Initial Assessment by a Physical Therapist
When a person with GBS begins physical therapy, the first step is a thorough evaluation.
Physical therapists assess muscle strength, flexibility, and functional mobility to understand the patient’s current abilities and limitations. This information is used to create a personalized treatment plan tailored to the patient’s specific needs and goals.
Initial evaluations and regular assessments using tools like the Timed Up and Go (TUG) test and the BERG Balance Scale help monitor progress and adjust therapy as needed.3
Timed Up and Go (TUG) Test
The TUG test is a quick and simple measure of a person’s mobility and balance. It involves timing how long it takes for someone to stand up from a chair, walk three meters, turn around, walk back, and sit down again. This test is often used to track the progress of patients with GBS.
BERG Balance Scale
The BERG Balance Scale is a widely used tool for evaluating balance and the risk of falling. It consists of 14 tasks, each scored on a scale from 0 to 4, with a maximum score of 56. Lower scores indicate a higher risk of falling, making this scale valuable for monitoring balance improvements in GBS patients over time.
Common Physical Therapy Treatments for Guillain-Barre Syndrome
In the early stages of treatment, known as the acute phase, physical therapists focus on supportive care. This includes positioning techniques to prevent pressure sores and contractures, as well as gentle range-of-motion exercises to maintain joint flexibility.
Even in this initial phase, keeping the body moving is important. Physical therapists may use gentle, passive exercises to help maintain flexibility and reduce stiffness without overexerting the patient.
As patients begin to recover and enter the recovery phase, the focus shifts to more active treatments. Physical therapists gradually introduce resistance exercises to rebuild muscle strength.
This process is carefully monitored to prevent fatigue and overuse. The BERG Balance Scale is frequently used to assess and improve balance. Balance exercises may include standing on one leg, walking a straight line, and other activities that challenge balance and coordination.
Functional mobility exercises are also an important part of recovery, helping patients regain their ability to perform everyday tasks.
The Timed Up and Go (TUG) test is valuable in this phase, as it provides a measurable way to track improvements in walking and transfers. All these exercises are tailored to the individual’s needs and abilities, progressively challenging the patient’s strength and endurance.2,3
Long-term Management for GBS
While Guillain-Barre Syndrome (GBS) can progress rapidly and be quite severe, many patients make a full recovery with the right treatment and rehabilitation. However, for many, the rehabilitation process continues even after leaving the hospital.
Continued physical therapy is often necessary to help patients regain full function and independence. Physical therapists work with patients to develop home exercise programs that support ongoing improvement.
Recovery can take weeks, months, or even years, and some individuals may experience lingering effects like weakness or fatigue. Some patients may need assistive devices, such as canes or walkers, to help with mobility. PTs can recommend and train patients to use these tools effectively.
Early intervention and comprehensive care are crucial for achieving the best possible outcomes for those affected by this challenging disorder. The road to recovery can be difficult, and emotional support is essential.
For this reason, PTs often collaborate with psychologists and counselors to address patients’ mental health needs, ensuring a holistic approach to care.
If you suspect that you may have GBS or any other neurological disorder, it’s important to contact your doctor as soon as you can.
Key Takeaways
- Guillain-Barré Syndrome is a rare condition where the immune system mistakenly attacks peripheral nerves, leading to symptoms like muscle weakness, tingling, and sometimes paralysis.
- The condition often follows infections such as respiratory or gastrointestinal illnesses; other triggers can include viral infections (e.g., COVID-19, flu), recent surgery, trauma, or, in rare cases, vaccinations.
- A neurologist typically diagnoses through clinical examinations, patient history, and specific tests like lumbar puncture, nerve conduction studies (NCS), and electromyography (EMG).
- A lumbar puncture can show elevated protein levels in cerebrospinal fluid, indicating nerve damage; NCS and EMG help determine the extent and type of nerve damage.
- Treatments include plasmapheresis (plasma exchange) and intravenous immunoglobulin (IVIG) therapy, which aim to reduce the immune system’s attack on the nerves and speed up recovery.
- Physical therapy is crucial in the recovery process, helping patients regain muscle strength, balance, and mobility. Initial assessments help create personalized treatment plans.
- In the acute phase, therapy focuses on supportive care, including positioning techniques and gentle range-of-motion exercises. The recovery phase introduces resistance exercises and balance training.
- Long-term management often involves continued physical therapy after hospital discharge, with some patients needing assistive devices like canes or walkers. Emotional support is also important for a full recovery.
FAQs
What are the main symptoms of Guillain-Barré Syndrome?
GBS typically begins with sudden muscle weakness and tingling sensations in the legs and feet. This weakness can quickly progress to the upper body and arms, sometimes within hours or days. Patients often describe a “pins-and-needles” sensation, which can escalate into severe muscle weakness or even paralysis. In the most severe cases, GBS can affect breathing muscles, leading to respiratory failure, a medical emergency requiring immediate attention.
What causes Guillain-Barré Syndrome?
The exact cause of GBS is not fully understood. It is believed to be triggered by an abnormal immune response, often following infections such as respiratory or gastrointestinal illnesses. Bacteria like Campylobacter jejuni, which causes gastroenteritis, are commonly linked to GBS. Viral infections, such as those caused by the flu, COVID-19, Zika virus, or Epstein-Barr virus, can also precede the onset of GBS. Other potential triggers include recent surgeries, trauma, or, in rare instances, vaccinations. However, the benefits of vaccinations generally far outweigh the risk of developing GBS.
How is Guillain-Barré Syndrome diagnosed?
GBS is diagnosed through a combination of clinical evaluation, patient history, and specific diagnostic tests. A neurologist will look for signs like muscle weakness, changes in reflexes, and sensory disturbances. Key diagnostic tests include lumbar puncture, which can reveal elevated protein levels in cerebrospinal fluid without an increase in white blood cells, and nerve conduction studies (NCS) and electromyography (EMG), which assess the speed and strength of electrical signals in the nerves and the electrical activity of muscles. These tests help confirm GBS by identifying characteristic patterns of nerve damage.
What treatments are available for Guillain-Barré Syndrome?
There is no cure for GBS, but several treatments can manage symptoms and aid recovery. Plasmapheresis (plasma exchange) involves removing and replacing harmful antibodies from the patient’s blood plasma, reducing the immune system’s attack on the nerves. Intravenous immunoglobulin (IVIG) therapy provides patients with healthy antibodies to neutralize the harmful ones, helping to suppress the immune response. Early intervention with these treatments can significantly improve outcomes and shorten the duration of the illness.
How does physical therapy help in recovering from GBS?
Physical therapy is a critical component of GBS rehabilitation. It helps patients regain strength, flexibility, and balance, promoting a gradual return to daily activities. Initial physical therapy often focuses on supportive care, such as positioning to prevent bed sores and gentle exercises to maintain joint flexibility. As patients progress, therapy includes more active interventions like resistance exercises to rebuild muscle strength and balance exercises to improve coordination. Regular assessments, using tools like the Timed Up and Go (TUG) test and the BERG Balance Scale, help track progress and adjust treatment plans.
Is full recovery possible from Guillain-Barré Syndrome?
Many individuals recover fully from GBS, although the timeline can vary widely. Recovery might take several weeks, months, or even years, depending on the severity of the case. Some patients may experience lingering symptoms like weakness, fatigue, or numbness. Early diagnosis and treatment are crucial for improving recovery outcomes. Ongoing physical therapy and, in some cases, psychological support can help patients regain their previous levels of function and well-being.
What kind of long-term care is needed for GBS patients?
Long-term care for GBS patients often involves continued physical therapy to regain full function and independence. Some may need assistive devices like canes or walkers, and therapists can provide training on their use. Additionally, because GBS can be a traumatic experience, emotional support and counseling are important aspects of recovery. Patients may benefit from working with psychologists or counselors to address mental health needs, ensuring a holistic approach to their overall well-being. In some cases, lifestyle modifications and home adaptations may also be recommended to support long-term recovery and improve quality of life.
References
- Willison, H. J., Jacobs, B. C., & van Doorn, P. A. (2016). Guillain-barre syndrome. The Lancet, 388(10045), 717-727.
- Bragazzi, N.L., Kolahi, AA., Nejadghaderi, S.A. et al. Global, regional, and national burden of Guillain–Barré syndrome and its underlying causes from 1990 to 2019. J Neuroinflammation 18, 264 (2021). https://doi.org/10.1186/s12974-021-02319-4
- Dimitrova, A., Izov, N., Maznev, I., Grigorova-Petrova, K., Lubenova, D., & Vasileva, D. (2017). Physical therapy and functional motor recovery in patient with Guillain-Barré Syndrome-Case report. European Scientific Journal, 13(33), 11-19.
- Plummer, Laura, PT, DPT, MS; Brown, Lisa, PT, DPT; Riley, Erin, PT, DPT. Guillain-Barré Syndrome. Monday, May 22, 2017. https://www.apta.org/patient-care/evidence-based-practice-resources/clinical-summaries/guillain-barre-syndrome
- Simatos Arsenault, N., Vincent, P. O., Yu, B. H. S., Bastien, R., & Sweeney, A. (2016). Influence of exercise on patients with Guillain-Barré syndrome: a systematic review. Physiotherapy Canada, 68(4), 367-376.





