Have you ever felt a sharp pain that started after exercise or a long walk? If the ache persists and worsens when applying pressure, you may have a stress fracture.
As a physical therapist who’s worked with many older adults recovering from a variety of fractures, I’m passionate about helping older adults understand, manage, and prevent stress fractures to maximize daily comfort and quality of life.
In this article, I will cover the symptoms of stress fractures, how they are diagnosed, and how they are managed. By the end of this article, I hope that you will feel more confident in your understanding of stress fractures to help minimize disability and make the best choices for your long-term health.
What Is a Stress Fracture?
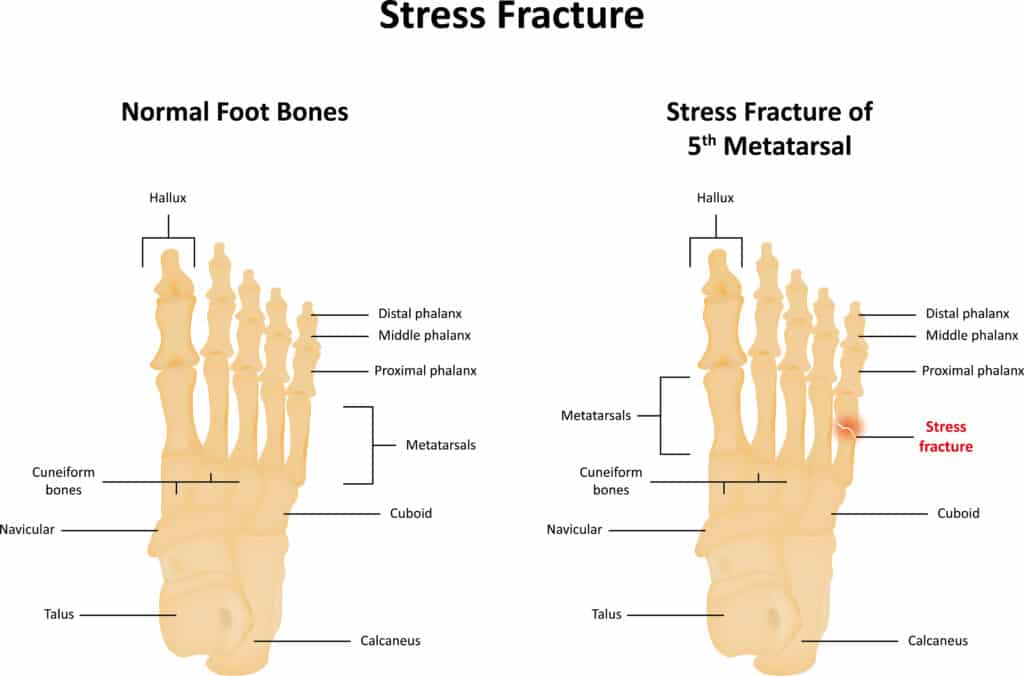
Stress fractures are small cracks in the bone due to repetitive stress or overuse.1
In most cases, you can think of a stress fracture as a slight hairline imperfection in the bone that may go unnoticed until it begins to cause pain. Unlike other types of fractures that usually result from a single traumatic event, such as a fall or a collision, stress fractures develop gradually over time during repetitive activities.
Stress fractures are common among older adults with weaker bones or who regularly perform high-impact activities like running, jumping, or dancing. Some of the risk factors for developing stress fractures include osteoporosis, poor nutrition, lack of rest, improper footwear, and sudden changes in exercise intensity.
In my experience working with older adults, the most common risk factor for stress fractures is osteoporosis or low bone density. With low bone density, even moderate or low-impact activities can result in stress fractures. For older adults with osteoporosis, focusing on managing osteoporosis should be the primary focus when aiming to prevent stress fractures.
What are the Symptoms of Stress Fractures?
Symptoms of stress fractures can vary based on their location and severity, but there are several common indicators to be aware of. These symptoms include:
- Pain: This is often the most noticeable symptom. The pain tends to intensify during physical activity and lessens with rest.
- Swelling, Tenderness, or Bruising: These symptoms may occur around the injured area, indicating a stress fracture.
- Difficulty in Weight-bearing: Experiencing challenges while walking or bearing weight on the affected limb is a common sign of a stress fracture.
- Restricted Joint Movement: There might be a limited range of motion or stiffness in the joints near the fracture site.
Stress fracture pain is distinct from other types of pain, such as the soreness that follows intense exercise or the discomfort associated with arthritis. Muscle soreness typically arises after new or rigorous physical activity and fades within a few days. Arthritis pain generally improves with mild physical activity.
In contrast, pain from a stress fracture is more localized and persistent and may not respond significantly to anti-inflammatory medications. Unlike muscle soreness or arthritis, stress fractures require a much longer healing time and do not resolve merely with rest and recovery.
In my clinical experience, the most frequent symptom observed in patients later diagnosed with stress fractures is pain during weight-bearing activities on the affected area, regardless of the position.
Common Locations of Stress Fracture
Stress fracture symptoms can also be specific to the fracture’s location. For instance, fractures in the feet might manifest as pain in the heel or foot arch, while a hip stress fracture could cause pain in the groin or buttock area.
In older adults, common sites for stress fractures include:
- Metatarsals: These are the long bones in the foot that connect to the toes.
- Tibia: Often referred to as the shin bone, the more prominent bone in the lower leg.
- Femoral Neck: Part of the thigh bone that connects to the hip; hip stress fractures often occur here.
- Vertebrae: In the spine, stress fractures are typically called compression fractures.
How are Stress Fractures Diagnosed?

Diagnosing stress fractures can be challenging, as they often don’t show up on standard X-rays in their initial stages. The reason for this is that X-rays typically reveal stress fractures only after they’ve caused significant bone damage, leading to noticeable gaps or deformities.
Even if you exhibit symptoms of a stress fracture and your X-ray results are clear, further testing might be necessary to verify the condition.
Here’s a summary of other key tests for detecting stress fractures beyond X-rays:
- Bone Scan: This nuclear imaging technique uses a small amount of radioactive material to illuminate areas of heightened bone activity. It can detect stress fractures two days post-injury and identify them in any body part.
- Magnetic Resonance Imaging (MRI): Using a strong magnetic field and radio waves, MRI creates detailed images of soft tissues and bones. It effectively identifies stress fractures as small regions of fluid or swelling within the bone marrow, providing insights into the injury’s severity.
- Computed Tomography (CT) Scan: A CT scan combines X-rays with computer technology to generate comprehensive body images. It can more precisely reveal stress fractures as slender cracks or lines in the bone.
From my experience, many stress fractures can be accurately identified using multi-angle X-rays. However, in cases where patients continue to experience symptoms despite negative X-ray results, an MRI is often employed for a more thorough evaluation.
If you suspect a stress fracture or if your symptoms intensify, it’s advisable to see a primary care physician or a physical therapist. They can conduct an examination and order appropriate tests to confirm the diagnosis, facilitating a quicker recovery and preventing complications.
How are Stress Fractures Treated?
The main goal of stress fracture treatment is to allow the bone to heal and prevent further damage. Your treatment options may vary depending on the specifics of your fracture. Still, they generally include some combination of the following:
Rest
Resting is the most critical first step in treating stress fractures. This means avoiding activities that cause pain or stress to the injured bone until it has healed adequately.
Depending on the fracture, this can take several weeks, so always follow your doctor’s advice on how long and how much you need to rest.
Inflammation Control
Applying ice to the injured area can help reduce pain and inflammation during the early stages of recovery. You can use an ice pack, a bag of frozen peas, or a towel wrapped around ice cubes for 10-20 minutes.
You may also be recommended to take anti-inflammatory medications by your doctor, which can help manage pain and inflammation symptoms when appropriately used.
Crutches or Braces
Using crutches or braces can help take some or all stress off the injured bone and allow it to heal correctly3.
Your doctor may recommend using crutches or braces depending on the location and severity of your stress fracture. For example, if you have a stress fracture in your foot or ankle, you may need to use a walking boot or a cast to immobilize the area.
If you have a stress fracture in your shin or thigh, you may need to use crutches to avoid putting pressure on the leg.
Physical Therapy
Physical therapy can help restore strength, mobility, and function to the injured area during and after healing4.
A physical therapist can design an individualized exercise program that suits your needs and improves your strength, balance, flexibility, and coordination.
The main goal of physical therapy is to optimize your physical function during recovery and give you the tools you need to prevent future stress fractures from happening.
What to Expect from Physical Therapy for Stress Fractures
I have worked with many patients during recovery from stress fractures, and the most common theme throughout physical therapy is to gradually increase activity and loading of the bone to promote complete healing. At the same time, nearby muscles must be strengthened to fortify the bone further, and education on managing and preventing fractures is a constant theme throughout therapy.
Patients commonly ask: “How do you know when a stress fracture is healed?” In most cases, this is done with more imaging after a set amount of time to determine if the bone defect has resolved.
Although rare, surgery may be required for severe or complicated stress fractures that do not heal with conservative treatment. Surgery may involve inserting screws, pins, plates, or rods to stabilize the bone and promote healing. It may also involve grafting bone from another part of your body or from a donor to fill in the gap or defect in the bone.
Like most physical conditions, surgery comes with a lot of risks, so it is usually reserved as a last resort when other treatments like rest, bracing, and physical therapy aren’t successful over a long period.
How can Stress Fractures be Prevented?

While stress fractures aren’t entirely preventable, you can take some simple steps to protect your bones and limit excessive stress on them. Here are a few practical tips on reducing the risk of stress fractures for older adults.
Proper Footwear
Choose shoes that fit well and offer sufficient cushioning to reduce stress on your feet and ankles during activities that involve heavy foot usage. Replacing your shoes regularly is essential as their ability to absorb shock can decrease over time.
Adequate Warm-Up
Before exercising, engage in light aerobic exercises, like dynamic leg and foot stretches. This preparation helps your muscles, tendons, and bones prepare for activity, thus preventing extra stress on your feet.
Gradual Increase in Physical Activity
When increasing your physical activity, do so gradually. A good rule of thumb is to increase the intensity and duration by no more than 10% per week. This approach helps avoid putting excessive stress on your bones, leading to stress fractures.
Balanced Diet
Consume a diet with plenty of calcium and vitamin D essential for strong bone health. Incorporate calcium-rich foods such as dairy products, leafy greens, nuts, and seeds, and ensure adequate vitamin D intake through sunlight exposure or foods like fatty fish and fortified milk.
Avoid Smoking and Excessive Alcohol
Smoking and heavy alcohol consumption can weaken your bones. Smoking reduces blood flow to the bones, affecting their healing capacity, while alcohol can interfere with the absorption of calcium and vitamin D, increasing the risk of bone density loss.
Regular Bone Density Tests
Especially for older adults, regular bone density tests are crucial. These tests help in monitoring bone health and early detection of osteoporosis, a condition that weakens bones and increases the risk of fractures.
In working with older adults to reduce the risk of stress fractures, I emphasize improving muscle and bone strength, promoting healthy dietary and supplement habits, and advocating for regular bone density testing.
Discussing your health history and activity goals with your primary care doctor to develop an effective plan for maintaining bone health is also beneficial.
Key Takeaways
- Stress fractures are small cracks in the bones due to repetitive stress or overuse.
- Stress fractures are common among older adults who have weaker bones or engage in high-impact activities.
- Stress fracture symptoms include pain, swelling, tenderness, bruising, and difficulty walking or bearing weight.
- Various tests, such as X-rays, bone scans, MRI, and C.T. scans can diagnose stress fractures.
- Stress fractures can be treated by resting, controlling inflammation, using crutches or braces, and engaging in physical therapy.
- Stress fractures can be prevented by choosing appropriate footwear, warming up properly before exercising, increasing physical activity gradually, eating a balanced diet, avoiding smoking and alcohol, and getting regular bone density tests.
References
- Carolina A. Moreira, John P. Bilezikian, Stress Fractures: Concepts and Therapeutics, The Journal of Clinical Endocrinology & Metabolism, Volume 102, Issue 2, 1 February 2017, Pages 525–534, https://doi.org/10.1210/jc.2016-2720
- Stress Fractures: Diagnosis, Treatment, and Prevention. American Family Physician. 2011;83(1):39-46.
- Splints and Casts: Indications and Methods. American Family Physician. 2009;80(5):491-499.
- Miller, T.L., Best, T.M. Taking a holistic approach to managing difficult stress fractures. J Orthop Surg Res 11, 98 (2016).
- Stress fractures: diagnosis and management in the primary care setting. Patrick G Robinson, Victoria BD Campbell, Andrew D Murray, Alastair Nicol, James RobsonBritish. Journal of General Practice 2019; 69 (681): 209-300. DOI: 10.3399/bjgp19X702137






