Arthritis is a common condition among active older adults, and it often leads to significant discomfort and pain, impacting daily life.
But the challenges posed by arthritis don’t have to be a constantly worsening concern. Physical therapy offers hope, providing effective pain management and improved mobility for many arthritis patients.
This comprehensive guide delves into the multifaceted role of physical therapy in arthritis care. From debunking common myths to exploring stretching, strengthening exercises, and innovative treatments, we uncover the transformative power of physical therapy in enhancing the quality of life for those with arthritis.
The Benefits & Key Components of Physical Therapy

Despite what you may have heard, arthritis isn’t inevitable with age, but it is still quite common. Thankfully, targeted physical therapy offers effective pain management when it does occur.
Relief from arthritis pain is a realistic goal, backed by research and clinical experience highlighting the benefits of exercises, stretches, and specific movement patterns used in physical therapy programs.
Physical therapy presents a focused strategy to alleviate arthritis-related discomfort, addressing pain through a holistic approach using a variety of reliable tools and techniques, including:
Joint Mobilization
Physical therapists use gentle techniques to mobilize and manipulate joints, reducing stiffness and pain. These techniques vary in intensity to enhance mobility and comfort. They can also be tailored to your needs, considering the severity of your arthritis.
Strengthening Exercises
Strengthening the muscles around affected joints is crucial for pain reduction. Stronger muscles support the joints, lessen strain, and subsequently decrease discomfort. Research confirms that stronger muscles around arthritic joints lead to less pain, especially during daily activities.
Pain-Relieving Modalities
Therapeutic methods like electrical stimulation (e.g., TENS) or heat/cold therapy are integrated into sessions to alleviate pain by boosting circulation and reducing inflammation. The choice of modality is customized to your arthritis condition and symptoms.
Physical therapy doesn’t just mask pain; it targets the root causes, offering a sustainable solution for managing arthritis pain. It empowers active older individuals with practical strategies, improving life quality and enabling a more active lifestyle despite arthritis challenges.
This approach is a testament to the role of physical therapy in enhancing the well-being of those with arthritis. Let’s explore the details of physical therapy to give you more insight into the difference it can make in your arthritis journey.
A Proven Method for Alleviating Arthritis Pain

Physical therapy is a practical, research-backed approach to managing arthritis pain, significantly enhancing the lives of those affected.
Research consistently highlights physical therapy’s crucial role in reducing arthritis discomfort. A critical study involving a comprehensive meta-analysis focused on the impact of strengthening exercises on osteoarthritis.
Participants engaging in these exercises saw improvements, but a more significant finding emerged. Those following a comprehensive exercise regimen designed by physical therapists experienced notable pain reduction. They also reported a better quality of life and improved functionality than the control group.1
Targeting Inflammation and Joint Dysfunction
Arthritis often presents a significant challenge to mobility, turning simple movements into daunting tasks. The inflammation and degeneration of joint tissues restrict smooth movement, leading to stiffness and difficulty in daily activities.
However, physical therapists specialize in exercises targeting these issues to improve flexibility and range of motion. Physical therapy exercises are carefully designed to enhance joint flexibility, leading to improved mobility.
These exercises, reflecting everyday movements, help boost coordination and ensure the regained mobility is practical for daily life. For those experiencing changes in walking patterns, physical therapy includes gait training to improve stability and walking mechanics.
This targeted approach makes physical therapy a vital tool in maintaining and enhancing mobility for those with arthritis. It offers a path to renewed independence and a better quality of life, showing that arthritis-related mobility challenges can be effectively managed.
Muscle Strengthening: A Key to Healthy Aging
Maintaining muscle strength is crucial as we age, especially for those with arthritis. Muscle-strengthening exercises not only manage arthritis effects but also boost overall health and vitality.
Strong muscles act as a buffer, mitigating arthritis’s impact on joints. Weak muscles exacerbate joint strain, increasing pain and instability. Recognizing this muscle strength-arthritis relationship is vital for effective treatment.
Strengthening muscles offers dual benefits for people living with arthritis: pain relief and enhanced joint support. This can significantly ease daily activities.
The upcoming sections will delve into various physical therapy exercises, providing practical examples to integrate into your routine in your journey toward healthy aging.
Related Content:
- How to Manage Arthritis: A Comprehensive Guide to Types, Symptoms, and Treatments
- Printable Lumbar Arthritis Exercises [PDF]
- An Active Adult’s Guide to AC Joint Arthritis
- Rheumatoid Arthritis Self-Care for Older Adults
- How Can Hand Therapy Help Me?
Targeted Exercise for Safeguarding Your Joints
Physical therapy plays a dual role in managing arthritis by addressing existing joint damage and as a preventative measure against further deterioration.
Arthritis typically involves gradually wearing down joint tissues like cartilage and synovium. This degradation can lead to bones rubbing together, causing pain and further joint damage. Understanding this process is vital for developing effective prevention strategies.
Physical therapy is proactive in preventing additional joint damage. Beyond symptom management, it focuses on preserving joint health and slowing arthritis progression.
Key to this approach is educating individuals on proper body mechanics. Physical therapists teach techniques to protect joints during daily activities, mitigating further damage risk.
Exercises that improve joint flexibility and maintain a healthy range of motion are central to this strategy. Physical therapists also guide individuals in choosing activities that support joint health and advise against those that could exacerbate symptoms.
By embracing physical therapy, individuals can be more active despite arthritis challenges. This approach extends beyond mere condition management, empowering individuals to maintain their health and well-being.
The Power of Stretching for Arthritis
Stretching is vital in managing arthritis and improving flexibility and joint range of motion. Regular stretching enhances muscle and tendon flexibility, aiding easier movement and reducing inflammation. It also relieves muscle tension, promoting relaxation in affected areas.
Static Stretching involves extending a muscle and holding the position, enhancing overall flexibility. A simple quadriceps stretch provides an excellent example of a static stretch to mitigate knee and hip pain.
Quadriceps Stretch
To do the chair quad stretch:
- Stand before a sturdy chair and place your left knee on the seat.
- Supporting your balance with a hand on the back of the chair, take a step forward with your right leg.
- Gently lean your hips forward until you feel a stretch in your left thigh.
- Hold for one minute, then repeat the stretch on the other leg.
Dynamic Stretching involves controlled, repetitive movements, ideal for warming up muscles to prepare your body for activity or to cool down after a workout. Here’s an example of one of our favorite dynamic stretches
Arm Swings
To do Arm Swings:
- Stand with your feet firmly planted hips-width distance apart.
- Begin to gently rotate at your waist, allowing your arms to freely swing as if trying to touch the opposite hip with each rotation.
- Swing for thirty seconds or more if it feels good.
- Note: Ensure you are in an open space where you can’t accidentally hit objects with your swinging hands.
Contract & Relax Stretching (Formally known as Proprioceptive Neuromuscular Facilitation, PNF) combines stretching and contracting muscles, and is ideal for after a hard workout. Here’s a great example for after a long jog, walk, or hike.
Hamstring Stretch
To do the contract and relax hamstring stretch:
- Place the heel of one foot on an elevated surface like a chair or park bench.
- Gently lean forward and rotate toward the outstretched leg, gently pressing your heel down into the surface for 3-5 seconds.
- Rotate back to the center, relaxing your leg. Repeat 8-10 times before switching legs.
Strengthening Exercises to Build Resilience
Targeted strengthening exercises improve muscle resilience, aiding arthritis management. These exercises decrease joint compression during movement, enhancing joint function.
Isometric Exercises are some of the most effective movements to boost strength and counter arthritis. These movements involve static muscle contractions, building strength without large joint movements. Quad sets are a classic example of isometric strength for knee health.
Quad Sets
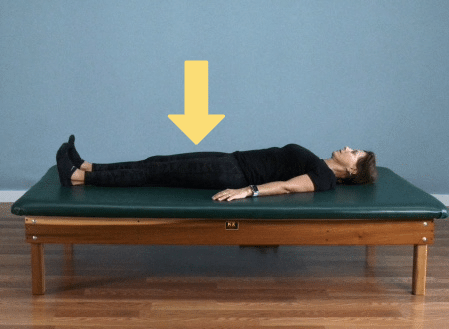
To do quad sets:
- Lie on a flat surface with your legs straight. This can also be done in a seated position with legs straight.
- Strongly engage the muscles in your thighs as if you are trying to straighten your leg maximally.
- Hold for five seconds, then relax. Repeat 10-15 times before switching legs.
Resistance Training involves using resistance bands or light weights to strengthen specific muscle groups. Wrist extensions are a classic strength movement for wrist arthritis.
Wrist Extensions
To do wrist extensions:
- Gripping a light hand weight (1-5 lbs.) or a small object roughly the same size and weight, place your forearm at the edge of a table. Your hand should reach off the edge with your palm facing down.
- Let the weight off your hand move down toward the floor as if you’re trying to reach your knuckles to the ground, then engage your forearm to move your hand toward the ceiling.
- This is can be a challenging exercise; continue the motion slowly with control until you feel fatigued in your hand and wrist, then switch hands and repeat.
Functional Strength Exercises Are key for integrating physical therapy exercises into daily activities. Examples include sit-to-stands and squats.
Sit to Stand
The perform a sit to stand:
- Sit upright at the edge of a chair with your feet flat on the floor.
- Leaning your body weight slightly forward, press through your feet to come to a tall standing position.
- Sit back down slowly, with control. Repeat for 10-20 repetitions or until you feel slightly fatigued. Rest and repeat.
Balance and Coordination Exercises
Balance and coordination exercises enhance stability, reducing risks associated with arthritis. Here are some examples that you can try at home:
Heel-to-Toe Walk
To perform a heel-to-toe walk:
- Begin standing with the toe of one foot touching the heel of the other
- Switch feet, as if you’re walking a tightrope. Using a line on the sidewalk or a piece of masking tape on the carpet may help.
- Walk from one end of the line to the other, heel to toe.
- Rest briefly, then turn around and repeat, focusing on unhurried, careful foot placement.
Single-Leg Stance
To perform a single leg stance:
- With a chair or another stable surface at your side for support, lift one leg off the floor. Try to maintain your balance for as long as possible, then repeat on the other leg.
- For variation, you can challenge yourself by setting a timer, and trying to beat your record on successive attempts. If you feel safe doing so, you can also attempt the activity with one or both eyes closed.
Note: if you have difficulty balancing, practice this exercise with your physical therapist before attempting it on your own.
Seated Marches on a Stability Ball
The do the seated ball march:
- Sit on a fully inflated stability ball with your feet flat on the floor. It’s also a good idea to stabilize the ball with both hands at your sides.
- Carefully lift one leg, then alternate, doing a slow march.
- Breathe deeply throughout the movement, completing 10 repetitions on each leg, then rest and repeat.
I recommend these exercises to my patients often, and they benefit a wide variety of people. Regardless, it’s best to schedule a consult with a physical therapist near you to target your specific needs and goals.
Massage & Electrical Stimulation: Effective Therapies for Arthritis Management
In a physical therapy program tailored for arthritis management, massage therapy and Transcutaneous Electrical Nerve Stimulation (TENS) can be helpful, enhancing the multifaceted approach to treatment.
These modalities are integrated with other therapeutic exercises to target the complex symptoms of arthritis, focusing on pain reduction and mobility improvement.
Massage therapy aids in alleviating muscle tension and joint stiffness, which is essential for preparing the body for other therapeutic activities. It boosts circulation, decreases inflammation, and increases range of motion, making daily tasks more manageable.
TENS adds a neurological dimension to pain management, employing electrical currents to disrupt pain signals and stimulate endorphin production. This method complements manual therapies and exercise, offering personalized pain relief that can be adjusted to the patient’s needs.
Massage and TENS represent a holistic approach within physical therapy for arthritis, aiming to ease symptoms and enhance overall quality of life.
This integrated strategy promotes active patient engagement in their treatment, leveraging a combination of techniques for a comprehensive management plan.
Tailoring Your Physical Therapy Journey: Timeline, Frequency and Monitoring Progress
The frequency and duration of physical therapy for older adults with arthritis vary based on individual needs, severity, and the treatment plan. General guidelines are:
- Frequency: Initially, sessions might occur two to three times weekly, focusing on symptom relief and exercise education. As improvement occurs and exercise proficiency increases, the frequency can decrease to weekly or longer.
- Duration: Sessions typically last 30 to 60 minutes, tailored to the individual’s tolerance and needs. The overall duration of therapy varies from weeks to months, depending on therapy goals, progress, and arthritis complexity.
Consistency is crucial in physical therapy. Regular participation in prescribed exercises, including at-home routines, is essential for therapy success.
These guidelines should be personalized, and a physical therapist will create a tailored plan based on individual assessment. Regular communication with the healthcare team ensures optimal therapy frequency and duration adjustment.
The Importance of Monitoring Progress
Monitoring your progress in physical therapy is a crucial part of managing arthritis. It helps you see how far you’ve come and what benefits you’re gaining, like finding daily tasks easier, feeling less pain, moving your joints more freely, and having more energy and endurance.
It’s not just about improving your physical health but also feeling better overall, which is a big win.
Keeping track of how you’re doing also helps your healthcare team. With attentive monitoring, doctors and PTs can see what’s best for you and adjust your therapy plan if needed. Plus, celebrating your improvements, big or small, can boost your motivation.
Recognizing these achievements is essential because they show the positive impact of your hard work in therapy. This makes the whole experience more rewarding and keeps you focused on reaching your goals.
The Transformative Power of Physical Therapy for Arthritis: A Case Study
This case study of my patient — we’ll call her Sarah — illustrates the profound impact of physical therapy on arthritis, particularly in the knees and hips.
When Sarah first consulted me, she struggled with intense pain that made simple tasks, like getting out of bed, extremely challenging. But her resilience was remarkable as she committed to a physical therapy program targeting her arthritis symptoms.
Sarah’s dedication to the exercise and stretching regimen was unwavering. The progress, though gradual, led to significant transformations.
Our sessions included exercises like sit-to-stands, mini squats, glute bridges, and core exercises in a high-kneel position, all aimed at strengthening Sarah’s muscles.
Significantly, Sarah noted a marked decrease in her morning pain and regained the ability to engage in activities she loved but had been hindered by arthritis. A notable milestone was her ability to play with her grandchildren on the floor and attend to her garden, activities she had previously found challenging.
Sarah’s experience underscores the effectiveness of tailored physical therapy in managing arthritis. It highlights how such treatment reduces pain and rejuvenates daily life activities. Her story is a compelling example that arthritis’s limitations can be overcome with determination and a strategic therapeutic approach.
Common Myths About Physical Therapy in Arthritis Management
Several myths about physical therapy (PT) and arthritis can lead to misunderstandings about its effectiveness and appropriateness. Let’s debunk some common misconceptions.
Myth: PT is Only for Severe Arthritis Cases
Reality: PT benefits all arthritis stages, not just severe ones. Early PT intervention can manage symptoms, improve function, and potentially slow arthritis progression.
Myth: PT Always Involves Painful Exercises
Reality: While some exercises may cause discomfort, PT isn’t about causing pain. Physical therapists customize programs to individual tolerances, balancing challenges, and manageability.
Myth: PT is Only About Stretching and Exercise
Reality: PT for arthritis includes more than exercises and stretching. It encompasses techniques like manual therapy, joint mobilization, pain-relieving modalities, and lifestyle education.
Myth: PT Doesn’t Work, Medications are Enough
Reality: Medications relieve symptoms, but PT addresses arthritis’s root causes. It improves joint function and muscle strength, enhancing well-being. Combining PT with medication often yields better results.
Myth: PT is Only for Younger Individuals
Reality: PT is effective for all ages, including older adults. Exercises are tailored to individual capabilities, ensuring safety and effectiveness.
Myth: PT is a Quick Fix
Reality: Physical therapy requires commitment and consistency. It’s a gradual process for building strength, improving flexibility, and enhancing function over time.
Debunking these myths promotes a better understanding of physical therapy’s benefits and versatility in arthritis management. PT is a customizable and valuable tool for improving the quality of life for individuals with arthritis.
Summary
In conclusion, physical therapy emerges as a vital tool in managing arthritis, transcending beyond mere pain relief to fundamentally improve joint function and overall well-being. Its multifaceted approach, encompassing joint mobilization, targeted exercises, and pain-relieving modalities, empowers individuals to regain mobility, strengthen muscles, and enhance their quality of life.
Regularly engaging in tailored physical therapy routines, both in clinical settings and at home, and monitoring progress plays a crucial role in overcoming the limitations of arthritis. This journey through physical therapy not only alleviates the physical symptoms of arthritis but also revitalizes the spirit, enabling individuals to lead more active, fulfilling lives.
Key Takeaways
- Physical therapy is effective at all stages of arthritis, not just in severe cases.
- It targets the root causes of arthritis pain, improving joint function and muscle strength.
- Techniques like joint mobilization, stretching, and strengthening exercises are vital components.
- Therapeutic methods such as electrical stimulation (TENS) and heat/cold therapy alleviate pain.
- Physical therapy enhances mobility, making daily tasks easier and improving quality of life.
- Regular participation in physical therapy, including at-home exercises, is crucial for success.
- Monitoring progress in physical therapy helps in refining treatment plans and maintaining motivation.
- Tailored physical therapy programs can significantly improve daily life activities and overall well-being.
- Dispelling common myths about physical therapy is essential for understanding its comprehensive benefits.
References
- Pelland, L., Brosseau, L., Wells, G., MacLeay, L., Lambert, J., Lamothe, C., … & Tugwell, P. (2004). Efficacy of strengthening exercises for osteoarthritis (part I): a meta-analysis. Physical therapy reviews, 9(2), 77-108.
- Resnick, B. (2001). Managing arthritis with exercise. Geriatric Nursing, 22(3), 143-150.
- Cairns, A. P., & McVeigh, J. G. (2009). A systematic review of the effects of dynamic exercise in rheumatoid arthritis. Rheumatology International, 30, 147-158.






