Most of us are familiar with the common symptoms of stroke, such as sudden numbness, confusion, or difficulty speaking. But do you know that strokes can also present in less obvious ways?
A stroke, sometimes referred to as a “brain attack,” occurs when — at least in the case of ischemic strokes — blood flow to an area of the brain is cut off, causing brain cells to die. This can lead to lasting damage, disability, or even death.
As a physical therapist, I’ve worked with many adults who have experienced a stroke and helped them during their recovery journey. While strokes are not uncommon, their effects can be minimized with early detection and treatment.
Understanding the signs and symptoms of severe health conditions like stroke becomes increasingly vital as we age.
In this article, we’ll explore some lesser-known stroke symptoms and offer practical advice on what to do about them. By staying informed and ready to respond, you can better protect yourself and others from the damage caused by a stroke.
The Basics of Understanding Stroke

In the most basic terms, a stroke is a medical emergency that occurs when the blood supply to part of your brain is interrupted, resulting in damage to brain cells. The effects of a stroke on the body and brain can be severe and permanent, depending on where and how severe the damage is.
These effects can range from mild to severe physical disability and memory and emotional difficulties. In some cases, they can be fatal.1
Having worked with many adults recovering from a stroke, I can confidently say that one of the most important factors is knowing the signs of a stroke to help get treatment faster.
Recognizing the Common Signs of a Stroke
There are a few tell-tale signs most commonly associated with a stroke. These include face drooping or numbness, especially on one side; arm weakness or numbness, often coupled with difficulty lifting the arm; and speech difficulties, such as slurring, inability to speak, or difficulty understanding speech. These symptoms often occur suddenly and can be obvious and alarming or somewhat subdued.
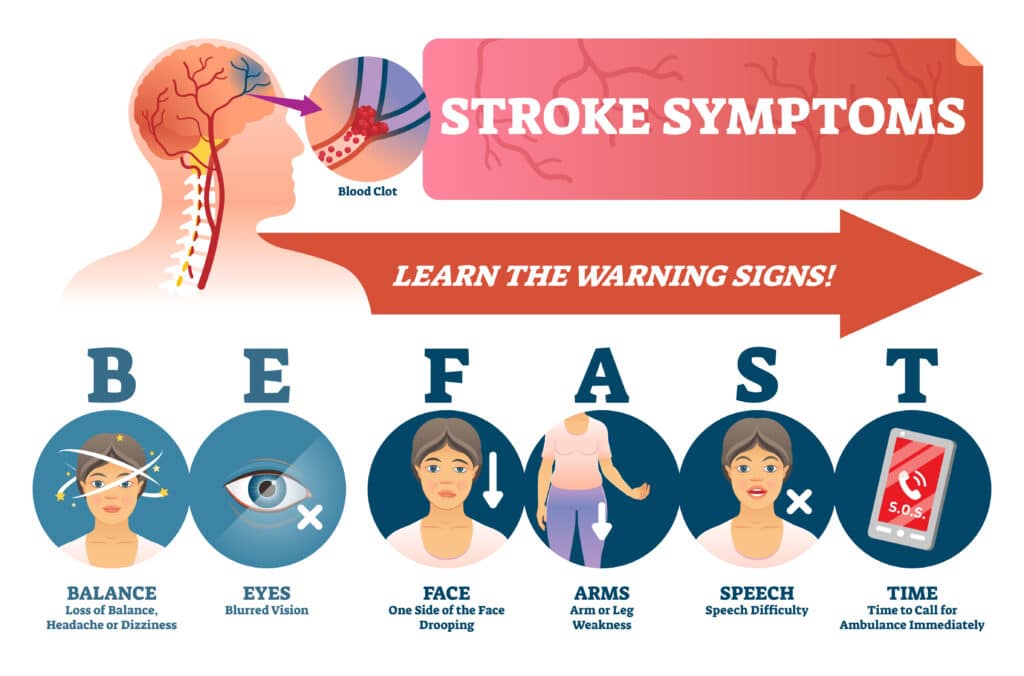
Remember the acronym BE FAST, a quick and effective way to remember the significant signs of a stroke:
- Balance: Are you experiencing a sudden loss of balance?
- Eyes: Is your vision doubled or blurry?
- Face: Does one side of the face droop?
- Arm: Is one arm weak or numb?
- Speech: Is speech slurred or hard to understand?
- Time: If you observe any of these signs, it’s time to call 911 immediately
These symptoms are the body’s signaling that something is seriously wrong. If you or someone around you experiences these symptoms, it is crucial to seek medical attention immediately. Every second counts regarding stroke treatment – the faster you get to a hospital, the more likely you are to minimize damage and have a better outcome.4
Many of the patients that I’ve worked with after a stroke had their stroke identified by a friend or family member – this means that you may be the person to recognize that your friend or family member is having a stroke and the person to call 911.
However, strokes can sometimes present with less common but equally important symptoms. These are often overlooked, ignored, or mistaken for other conditions, delaying necessary, time-sensitive treatment.
Unusual Stroke Symptoms You Shouldn’t Ignore
A stroke is a serious medical condition that requires immediate attention. However, its symptoms can often be mistaken for other health issues, leading to a delay in treatment.
This is because some stroke symptoms are considered unusual and not widely known. Understanding and recognizing these lesser-known makes getting immediate help and preventing further complications easier.
Sudden Dizziness, Loss of Balance, or Trouble Walking
A stroke can affect the brain’s ability to coordinate movement, resulting in dizziness, loss of balance, or trouble walking.5
If you suddenly feel dizzy or lose your balance, it cannot be dismissed as mere fatigue or aging. These could be signs of a stroke.
Sudden Vision Problems in One or Both Eyes
Another unusual symptom of a stroke is sudden vision problems. You may experience blurred vision, double vision, or even blindness in one or both eyes.
These vision issues occur when a stroke interferes with the part of the brain that controls our eye movements and visual processing.
While gradual changes to your eyesight are important to address and should be looked at by a trained professional as you notice them, vision problems caused by a stroke are sudden and often profound. If your vision changes suddenly, get help immediately.
Sudden Severe Headache with No Known Cause
A sudden, severe headache with no apparent cause could be a warning sign of a stroke. This type of headache is often intense, unlike any headache you’ve had before, and it can occur without any other typical stroke symptoms.6
Sudden Nausea, Vomiting, or Hiccups
Surprisingly, sudden nausea, vomiting, or hiccups can also be a sign of a stroke.
Although these symptoms are less common, they can occur when a stroke affects the base of the brain, where the centers for vomiting and hiccupping are located.7
The Importance of Recognizing Symptoms and Acting Fast

Early identification of these unusual stroke symptoms can significantly increase the chances of successful recovery—every minute counts when it comes to stroke treatment. The sooner medical intervention is initiated, the better the outcome.
It’s critical to remember that these symptoms often appear suddenly and without warning. If you experience any of these symptoms, seek immediate medical attention, even if the symptoms seem to go away. It’s always better to be safe than sorry when considering the health of your brain.
Spotting Unusual Stroke Symptoms for At-Risk Groups
When it comes to the symptoms of a stroke, different factors like age, gender, and certain health conditions can change how a stroke presents itself. Let’s cover a few examples to help you feel prepared to catch these symptoms early.
Stroke Symptoms in Women
Women may experience stroke symptoms that are more subtle or vague than those typically associated with stroke. This can be due to things like hormonal changes, pregnancy, and the use of some birth control medications, which may increase a woman’s risk of stroke.8
In addition to the common signs of a stroke, women can experience chest pain, sudden shortness of breath, or heart palpitations. Behavioral changes, such as sudden agitation or mood swings, can also occur. Unusual physical symptoms may include pain in the face, arm, leg, or abdomen.9
Stroke Symptoms in Older Adults
Aging increases our risk of stroke, especially after the age of 65. This is typically because older adults often have more pre-existing conditions, such as high blood pressure, diabetes, or heart disease, which further increase the risk of significant medical events like stroke.
When an older adult experiences a stroke, the symptoms may lean more toward cognitive or emotional changes. For example, they may display memory loss, confusion, or disorientation.
They might also show changes in mood, such as depression, apathy, or a lack of interest. More extreme personality changes, such as paranoia or impulsiveness, can also be signs of a stroke.
Common Health Conditions That Increase Stroke Risk
Certain health conditions, particularly heart disease and diabetes, significantly elevate the risk of stroke. Heart diseases, such as atrial fibrillation and heart valve defects, often lead to the formation of blood clots in the heart, which can then travel to the brain and cause a stroke.
Similarly, both Type 1 and Type 2 diabetes heighten stroke risk due to the potential damage high blood sugar levels can cause to blood vessels and nerves.
Managing these conditions is critical for reducing stroke risk. For heart disease, this may involve regular cardiac monitoring, medications like blood thinners and lifestyle changes to support heart health. For diabetes, controlling blood sugar levels through diet, exercise, and medication is key.
Regular medical check-ups are essential for both conditions to monitor and manage any changes that could increase stroke risk.
Spotting Unusual Stroke Symptoms & Varieties

Some varieties of stroke are less common and, as a result, are less well known. Here are two unusual stroke varieties and the symptoms to watch out for:
Eye Stroke: A Rare Condition with Unusual Symptoms
Eye stroke, or retinal artery occlusion, is a rare stroke that directly affects vision. It disrupts the blood supply to the retina, the area in the back of the eye that captures light. The most notable symptom of an eye stroke is sudden, painless vision loss in one eye, which can be partial or complete.
One of my previous patients is a survivor of an eye stroke. While he was not experiencing any other symptoms, he was still immediately seen for treatment and monitored in the hospital for several days. This is because an eye stroke can be a warning sign of a more significant stroke in the brain, which needs to be treated quickly to prevent permanent vision loss or blindness.
Spinal Stroke: Uncommon but Noteworthy
Just as an eye stroke affects vision, a spinal stroke affects our body’s movements. Put simply, spinal stroke is another rare type of stroke that disrupts the blood supply to the spinal cord.
The hallmark symptom of a spinal stroke is sudden, severe back or neck pain, followed by numbness or weakness below the level of the injury. Like any other type of stroke, a spinal stroke requires immediate medical attention to prevent further damage or complications.
Keep in mind that each person is unique, and stroke symptoms can vary dramatically from person to person. If you or a loved one experiences any unusual symptoms, don’t hesitate to seek immediate medical help. Remember, a quick reaction equates to a life saved, and early treatment can make a significant difference in recovery.
Understanding Stages of Stroke Treatment
Factors such as the severity of the stroke, overall health, and motivation significantly shape the recovery journey.
But before delving into the recovery process, it’s essential to understand what happens during the critical phase of acute stroke care, as prompt and appropriate treatment can vastly improve outcomes.
Acute Stroke Care: The First Steps
When a stroke is suspected, an immediate medical response is vital. Since most strokes are ischemic, getting treatment within three hours of symptom onset allows for the use of specialized medicines, leading to more positive outcomes.
Immediately calling 911 when stroke symptoms are recognized ensures that emergency medical services can provide life-saving care en route to the hospital. This often includes directing the patient to specialized stroke centers for prompt treatment.
Upon arrival at the hospital, the medical team conducts a thorough assessment, including reviewing the patient’s medical history and determining when the symptoms started. Brain imaging, such as CT scans or MRIs, is crucial to identify the type of stroke – ischemic (caused by a clot) or hemorrhagic (caused by bleeding).
Treatment varies based on the stroke type. For ischemic strokes, swift administration of clot-dissolving medications like tPA (Tissue Plasminogen Activator) within a three-hour window can be life-saving.
In cases of hemorrhagic stroke, the focus shifts to controlling bleeding and reducing pressure in the brain, which may involve medications, surgery, or endovascular procedures.
Rehabilitation and Beyond
Rehabilitation typically begins in the hospital as soon as it’s safe, sometimes as early as a day or two after the stroke. The aim is to facilitate the transition home and reduce the risk of another stroke.
Recovery can range from a total return to pre-stroke functions to enduring some level of disability. Rehabilitation efforts are tailored to individual needs, encompassing physical, speech, and occupational therapies.
Long-term management is equally crucial. Addressing underlying health issues like heart disease, hypertension, or diabetes is essential in preventing future strokes. Lifestyle changes, medications, and possibly surgery form part of a comprehensive stroke prevention strategy.
The Role of Therapy in Stroke Recovery
Generally, post-stroke, the path to regaining lost skills involves various types of therapy. These include physical, occupational, speech, and cognitive therapy. Each type of therapy serves a specific purpose in the recovery process.
For instance, physical therapy helps improve muscle strength and coordination, which is vital for regaining mobility.
Conversely, occupational therapy focuses on improving daily activities such as eating, dressing, and bathing. Speech therapy aids in regaining lost speaking abilities, while cognitive therapy helps with memory, attention, and problem-solving skills.
Having helped patients who are recovering from stroke through their physical therapy, I can attest to how unique each person’s recovery process truly is. From week to week and even day to day, treatment goals can change drastically depending on the most pressing symptoms and physical skills that require the most work.
Lifestyle Modifications for Stroke Prevention

As a physical therapist, I’ve observed firsthand how crucial lifestyle changes are in reducing the risk of strokes. Here a few of the key areas to address when focusing on stroke prevention:
Managing Blood Pressure, Cholesterol, and Blood Sugar
High blood pressure, cholesterol, and uncontrolled blood sugar are significant stroke risk factors. If necessary, regular monitoring and management through diet, exercise, and medication are essential.
This includes reducing sodium intake, avoiding high-cholesterol foods, and maintaining healthy blood sugar levels, especially for people with diabetes.
Quitting Smoking and Limiting Alcohol
Smoking and excessive alcohol consumption both increase stroke risk. Quitting smoking is one of the most effective measures, with immediate health benefits. Similarly, moderating alcohol intake is vital, ideally limiting it to one drink per day for women and two for men.
Regular Exercise and Healthy Diet
Regular physical activity, such as brisk walking or cycling, and maintaining a balanced diet of fruits, vegetables, and whole grains significantly reduces stroke risk.
Exercise also aids in maintaining a healthy weight, which is crucial in preventing strokes.
Routine Health Check-ups
Regular check-ups are essential for early detection and managing stroke risk factors. They ensure timely intervention for any health concerns that could increase stroke risk.
Incorporating these lifestyle modifications lowers the risk of stroke and enhances overall health and well-being. As individuals, we have the power to make choices every day that can lead to a healthier life and significantly lower our stroke risk.
Navigating Stroke Recovery
Living after a stroke brings unique challenges and opportunities for recovery and adaptation. The journey is highly individual, but several common elements are crucial in enhancing the quality of life and facilitating recovery for those affected. Alongside the therapies mentioned above, here are some areas of attention.
Emotional and Psychological Support
Recovering from a stroke is not just a physical process. The emotional and psychological impact can be significant. Support from family, friends, healthcare professionals, and support groups is crucial. Counseling or therapy can also be beneficial in dealing with the emotional aftermath of a stroke.
Lifestyle Adjustments
Post-stroke, it’s often necessary to make lifestyle changes to prevent future strokes and manage ongoing health. This might include dietary changes, regular exercise appropriate for the individual’s abilities, and continued management of medical conditions like hypertension or diabetes.
Adapting the Living Environment
Making modifications to the living environment can significantly improve safety and independence. This may involve installing grab bars in the bathroom, using assistive devices for mobility, or rearranging furniture to accommodate mobility limitations.
Community Resources and Support
Leveraging community resources like stroke survivor groups, rehabilitation centers, and home health services can provide additional support. Many communities offer programs specifically designed for stroke survivors, which can be invaluable in recovery.
Staying Engaged and Active
Engagement in meaningful activities and hobbies is important for mental well-being. It’s beneficial for stroke survivors to stay as active and involved as possible through social activities, hobbies, or volunteering.
By addressing these aspects, individuals who have experienced a stroke can recover more effectively and improve their overall quality of life.
In my practice, I emphasize the importance of a holistic approach to post-stroke living, encompassing physical recovery, emotional well-being, and lifestyle adjustments. Taking the health of your brain and body seriously is the most effective way to ensure the best possible outcomes for stroke survivors.
Key Takeaways
- Recognizing stroke symptoms early is essential, leading to more effective treatment.
- Common stroke symptoms include facial drooping, arm weakness, and speech difficulty, which are critical indicators.
- Strokes can also present with less common symptoms like sudden confusion, dizziness, and severe headaches.
- Immediate medical assistance is crucial and can significantly improve the chances of recovery from a stroke.
- Stroke symptoms can vary based on gender and age, with women and older adults experiencing unique signs.
- Effective acute stroke care involves a rapid emergency response, accurate hospital diagnosis, and appropriate treatment.
- Recovery from a stroke is highly personalized, involving different types of therapies such as physical, occupational, speech, and cognitive therapy.
- Lifestyle modifications, including managing blood pressure and quitting smoking, are essential in preventing strokes.
- Emotional and psychological support plays a crucial role in the recovery process after a stroke.
- Controlling blood pressure, cholesterol, and blood sugar, along with regular exercise and emotional support, can help prevent strokes and aid recovery.
FAQs
What is a stroke, and why is it sometimes referred to as a “brain attack”?
A stroke occurs when the blood supply to a portion of the brain is interrupted, either by a blockage (ischemic stroke) or bleeding (hemorrhagic stroke). This interruption deprives brain cells of oxygen, leading to cell death and potentially causing long-term damage. It’s called a “brain attack” because, similar to a heart attack, it’s an urgent medical condition that requires immediate attention. If not treated promptly, a stroke can lead to severe disabilities or even death, but quick medical intervention can minimize the damage and improve recovery outcomes.
What are the most common symptoms of a stroke, and how can I recognize them?
The most common signs of a stroke are sudden onset and may include facial drooping (especially on one side), arm weakness or numbness (making it difficult to lift or control one arm), and speech difficulties (such as slurred speech or inability to speak or understand others). A helpful way to remember these signs is with the acronym BE FAST:
• Balance: A sudden loss of balance or coordination.
• Eyes: Blurred or double vision, or sudden blindness in one or both eyes.
• Face: One side of the face droops or feels numb, often visible when smiling.
• Arms: One arm becomes weak or numb, and you may not be able to raise it fully.
• Speech: Speech becomes slurred, or you have difficulty speaking or understanding.
• Time: If you notice any of these signs, call 911 immediately. Time is critical, as treatment within the first few hours can significantly reduce brain damage and improve recovery prospects.
Can strokes present unusual symptoms, and what should I look out for?
Yes, in addition to the classic symptoms, strokes can also present with less common signs that are easily mistaken for other conditions. These include sudden dizziness, loss of balance or coordination, severe headache (which may feel unlike any headache you’ve had before), and vision problems such as double vision, blurry vision, or sudden blindness. Some people may also experience nausea, vomiting, or hiccups, particularly if the stroke affects the base of the brain. It’s important not to dismiss these symptoms, especially if they appear suddenly. Seeking immediate medical attention could make the difference in preventing long-term damage or death.
How do stroke symptoms differ in women and older adults, and why is it important to recognize these differences?
In women, stroke symptoms may sometimes appear more subtly and be mistaken for other conditions. Along with the traditional symptoms, women may also experience less common signs like chest pain, shortness of breath, heart palpitations, or unexplained pain in areas such as the face, arm, leg, or abdomen. They may also exhibit sudden mood swings, agitation, or behavioral changes, which can be misinterpreted as emotional issues rather than signs of a stroke.
For older adults, symptoms may lean more toward cognitive and emotional changes. Memory loss, confusion, disorientation, or dramatic mood shifts (such as sudden depression, apathy, or paranoia) can occur, sometimes without the typical physical symptoms. Because older adults are more likely to have underlying health conditions like high blood pressure, heart disease, or diabetes, recognizing these non-physical signs is crucial for timely stroke intervention and prevention.
What can I do to reduce my risk of having a stroke, and what lifestyle changes should I consider?
Several risk factors can increase your chances of having a stroke, but managing certain health conditions and adopting healthier habits can significantly reduce your risk. First and foremost, controlling high blood pressure, cholesterol, and blood sugar levels is essential. This can involve taking prescribed medications, reducing sodium and fat intake, and maintaining a balanced diet rich in fruits, vegetables, and whole grains.
Quitting smoking is one of the most effective ways to lower your stroke risk, as smoking damages blood vessels and increases the likelihood of clot formation. Limiting alcohol intake is also important, with recommended guidelines suggesting no more than one drink per day for women and two for men. Regular exercise, such as walking, cycling, or swimming, helps maintain a healthy weight and supports heart health, reducing the risk of stroke.
What should I do if I suspect someone is having a stroke?
If you suspect someone is having a stroke, call 911 immediately. It’s vital not to wait or dismiss the symptoms, as time is of the essence in stroke treatment. While waiting for emergency services, keep the person calm and comfortable, and make sure they don’t eat or drink anything, as swallowing may be impaired. Observing their symptoms can help medical professionals identify the type of stroke they are experiencing and provide the right treatment as soon as possible.
Recognizing a stroke quickly and getting medical help can greatly improve the person’s chances of recovery and minimize long-term damage.
References
- American Stroke Association. Stroke Symptoms.
- National Institute of Neurological Disorders and Stroke. Know Stroke.
- Harvard Health Publishing. Act FAST to Recognize a Stroke in Progress.
- National Institute of Neurological Disorders and Stroke. (2021). Stroke Information Page. National Institutes of Health.
- American Heart Association. (2020). Stroke, TIA, and Warning Signs.
- Stroke Association UK. (2020). What is Stroke.
- American Stroke Association. (2021). About Stroke.
- Lisabeth L, Bushnell C. Stroke risk in women: the role of menopause and hormone therapy [published correction appears in Lancet Neurol. 2012 Feb;11(2):125]. Lancet Neurol. 2012;11(1):82-91.
- Di Carlo A, Lamassa M, Baldereschi M, et al. Sex differences in the clinical presentation, resource use, and 3-month outcome of acute stroke in Europe: data from a multicenter multinational hospital-based registry. Stroke. 2003;34(5):1114-1119.
- Boehme AK, Esenwa C, Elkind MS. Stroke Risk Factors, Genetics, and Prevention. Circ Res. 2017;120(3):472-495.